Dr. Gregory Hickman, the medical director and anesthesia director at the Andrews Institute Ambulatory Surgery Center in Florida recently shared his master tips for performing ultrasound-guided injections during a webinar hosted by Clarius, The Mobile RA: Using Handheld Ultrasound to Guide PEC and Supraclavicular Blocks Plus Intra-Articular Injections.
Watch the recording of the full webinar at your convenience. Or for a short synopsis, read the following best practices by Dr. Hickman’s for performing an intra-articular injection of the knee.
Indications for Intra-Articular Injection of the Knee
“This is an injection I do in the operating room. Almost all of our knee arthroscopies are done under general anesthesia, so we can do a knee injection right after induction, and it has time to work by the time the patient is prepped and draped and the surgeon gets started.
We use them with knee arthroscopies that are doing debridement, meniscectomy and meniscus repair, chondroplasty, and for microfractures.
There are Many Benefits to Intra-Articular Injections of the Knee
This is a low-risk procedure with a really high reward and we’ve seen great results for many years. We combine this injection with a multimodal approach because it:
- Decreases our postop narcotics use in the PACU,
- Decreases multiple side effects from opioids,
- Decreases our PACU time,
- Increases ASC throughput, and
- Increases our patient satisfaction.
This Multimodal Approach Hits Different Parts of the Nervous System and Reduces Narcotic Use
Following are some of our typical doses.
- Preoperatively: a gram of acetaminophen
- Under general anesthesia:
- Ketorolac 30 milligrams
- Ketamine 15 milligrams
- Fentanyl 2 cc
- For anti-inflammatory effects: 4 to 8 milligrams of dexamethasone in our intra-articular injection
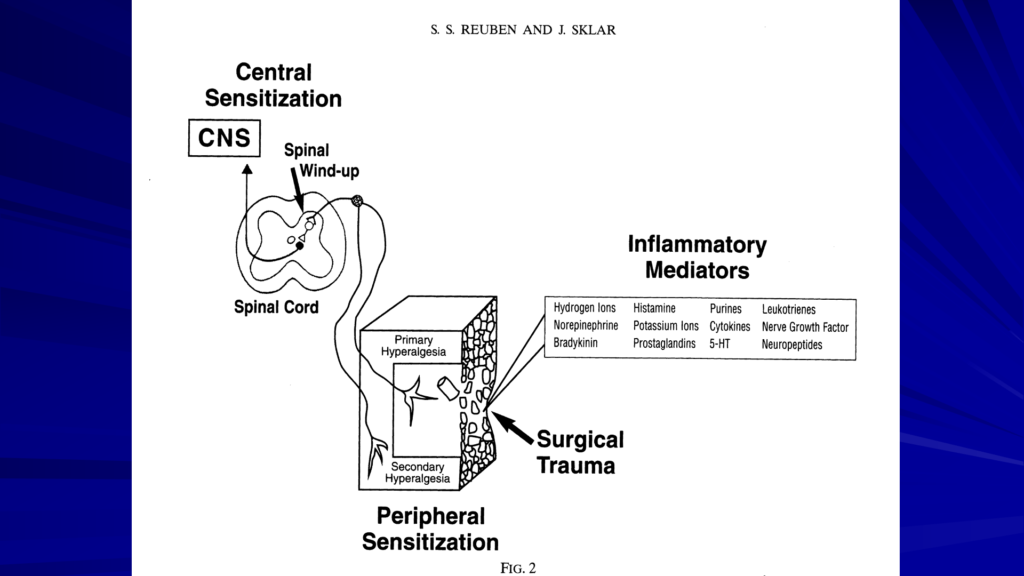
Tylenol works centrally in the brain. Ketamine works in the posterior lateral horn of the spinal cord. Our dexamethasone and Ketorolac combo works as anti-inflammatories. And so, with a multimodal approach, we’re hitting different parts of the nervous system to prevent the pain from ever reaching the brain. The published theory is that if we prevent different parts of the nervous system from firing and prevent the spinal lined up, then we can greatly reduce our narcotic needs in the recovery room. In practice, it’s working well for us and our patients.
Opioid Receptors are on Peripheral Nerves and Work in the Knee Joint
We know that opioids work on mu, kappa, delta and sigma receptors. We’re also aware that opioid receptors are out on peripheral nerves. So, when we’re putting it in the knee, in the joint, it actually works there in the periphery.
For an intra-articular injection of the knee, I usually use 30 cc of bupivacaine and primarily use 10 milligrams of morphine. A couple years ago, we had trouble getting morphine. So, I switched to Meperidine and use 100 milligrams. Meperidine, if you look at the chemical structure, is actually pretty similar to local anesthetics. And there are some thoughts that it may actually have some local anesthetic effect also.
With bupivacaine, we used to always use with epinephrine. We’ve had trouble getting the bupivacaine with epinephrine in the last couple of years. So, we’re using it plain without it. We use either one. I like epinephrine, but if we can’t get it, we just use the plain bupivacaine.
It’s a Low Risk Procedure with Excellent Results
In the last 25 years or so, I’ve done close to 30,000 of these intra-articular injections on knee arthroscopies. We’ve seen no infections, basically, no bleeding problems, and no local anesthetic toxicity. It’s a low-risk procedure.
We have never had any issues with chondrolysis or any problems with the cartilage in our knee arthroscopies. It’s not an issue because we’re not getting prolonged exposure to the local anesthetic.

Looking at the patella in the image above, we’re doing our injection at the dot, on the lateral aspect, superior lateral aspect of the patella.
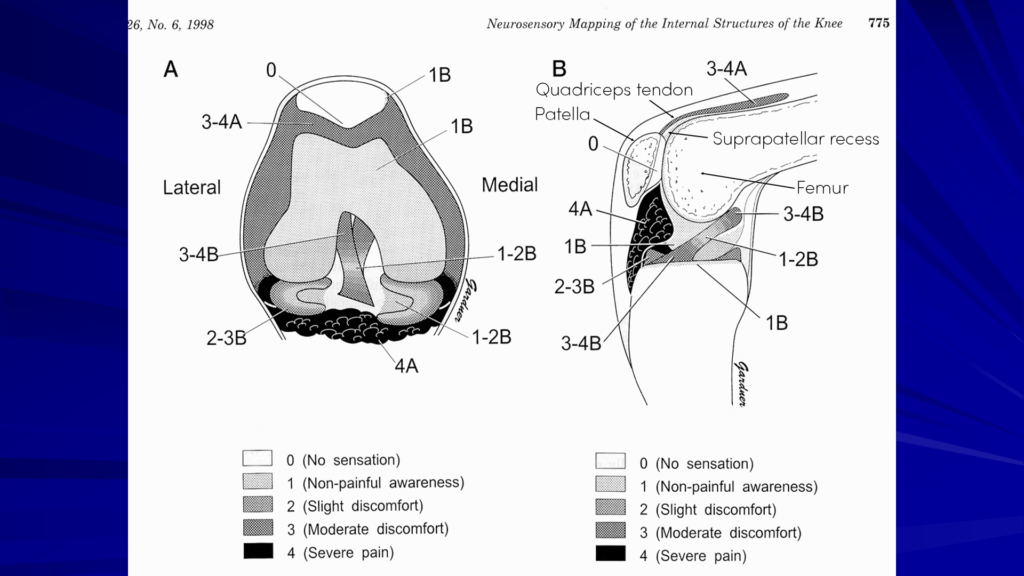
Looking at this drawing, we’re coming up into the suprapatellar recess, just under the quadriceps tendon and between the femur. If we inject just in this area (3-4A), that local is going to spread all down into the joint. It’s going to get into the meniscal, the fat pads, and the ACL and PCL. So, it gets a really good spread throughout the joint for about 10 to 15 minutes, until they start the surgery.
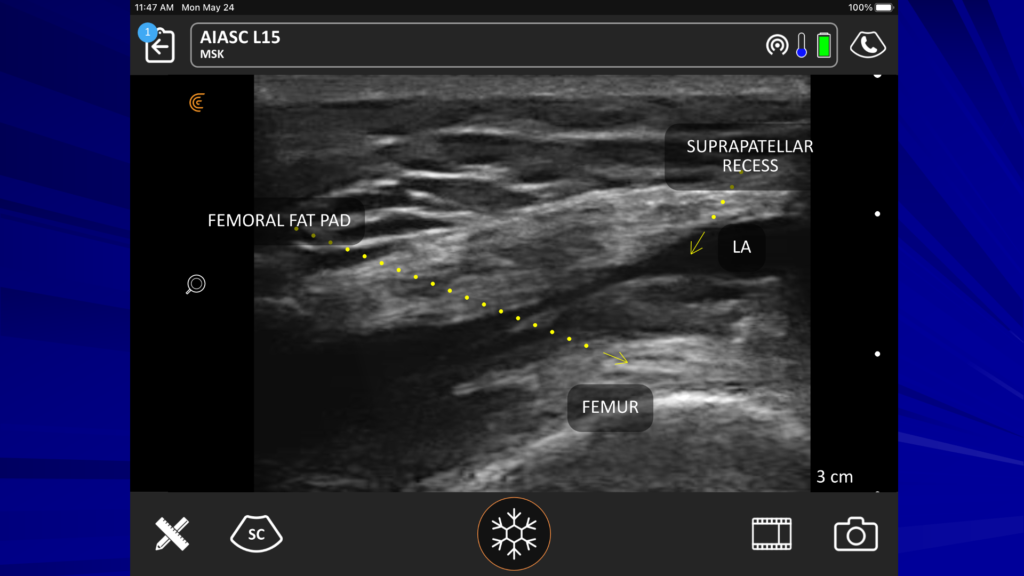
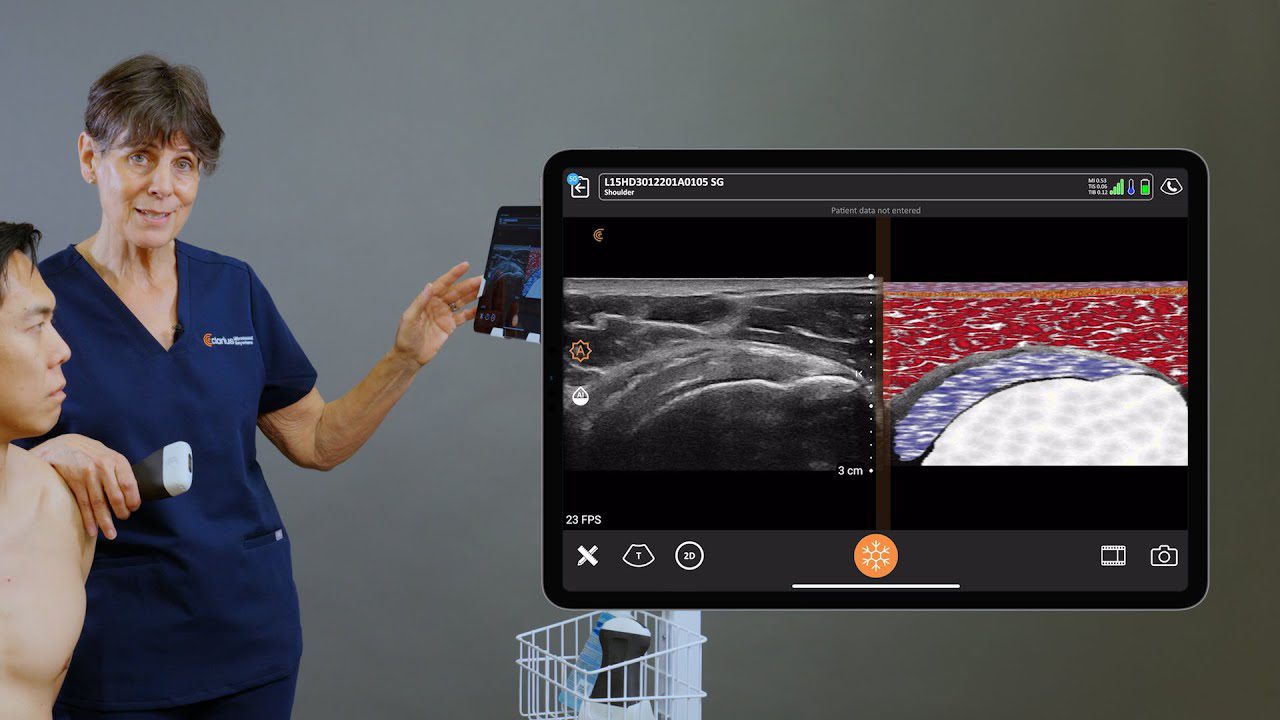
On the ultrasound image above, you see our suprapatellar recess. We have our femur, our femoral fat pad and just above that, we have the recess we’re looking to get into. And when you inject, you won’t see this move much. All the local will go down nicely into the joint.
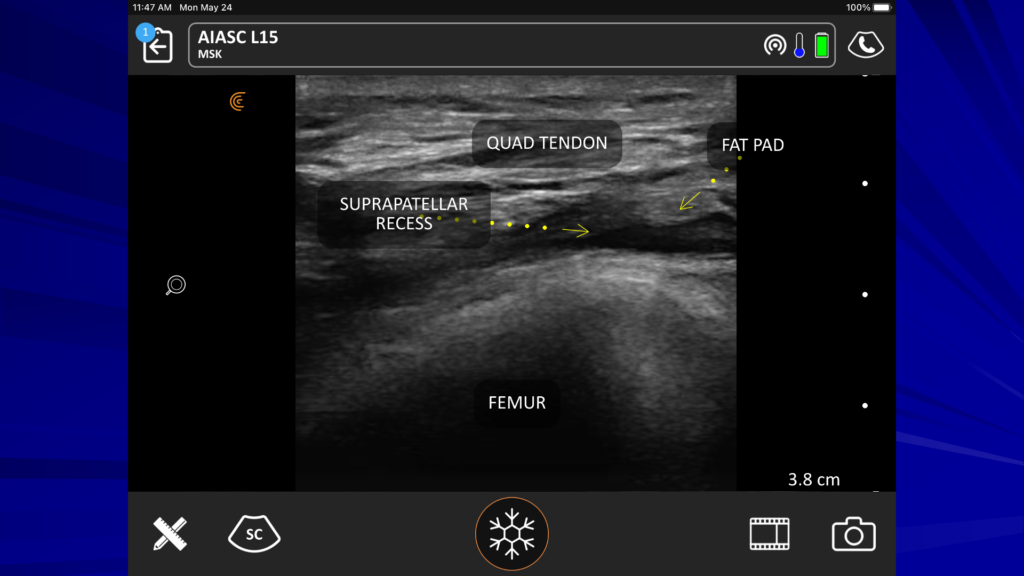
Here’s another picture to give you another idea of the little space we’re looking at just above the femur – we’re just proximal to the patella.

One more look: you can see that we’re trying to get our needle into this really small suprapatellar recess. We come in from the lateral aspect.
A Video Demonstration of the Intra-Articular Injection
In the following video, you see me coming in lateral, flat parallel to the probe. You can see our probe is easy to use. You should see the needle really well coming in from the right side of the screen on the iPad. You won’t see the local open-up space. I’ve injected 30 cc in there, and it didn’t open up at all. So, you know it went into the joint very well.
It’s a big potential space and has a good access point that flows right into the joint. If somebody has a big effusion, the suprapatellar recess will be wide open.
A Low Risk and Successful Procedure that’s Growing in Popularity!
This is a procedure that can be done on an awake patients because it doesn’t cause pain when done under ultrasound guidance. Injecting blindly into the knee could cause us and our patients both a lot of aggravation if scrape the patella or hit the femur while trying to find the joint. With ultrasound, it’s satisfying to glide in painlessly.
I’ve been doing this injection a long time and presented a paper on it at ASRA in 2000 or 2001. I hope that sharing my success will continue to help this procedure grow in popularity. My recovering nurses really see a big improvement with recovery. I know it works just because they tell me.”
How Dr. Hickman Uses Clarius HD
As co-founder of the popular ultrasound-guided regional anesthesia education website, blockjocks.com, Dr. Hickman is well versed in teaching his techniques to clinicians around the world. He has been using Clarius handheld ultrasound since it was first introduced in 2016. He currently uses the Clarius L7 HD to guide nerve blocks, including femoral blocks and adductor canal blocks.
One thing I love about Clarius is the mobility,” he explains. “If I need to go over to PT, and we do a lot of continuous catheters, it’s great to have portable ultrasound. And so, if we have a catheter in a patient who is in PT and they’re not doing as well, we can go over and just check the catheter location. It’s really easy. We can just inject some local through the catheter and see the spread around the nerves. It’s so easy to grab the iPad and the probe and walk over for a check. It’s really quick and really easy to do.”
Interested in Using Clarius Ultrasound for Your Regional Anesthesia Practice?
Wireless and pocket-sized, Clarius scanners deliver the high-definition imaging and power you expect from a traditional ultrasound system in a highly affordable ultra-mobile scanner. Visit our regional anesthesia specialty page to learn more about Clarius. Or book a demo for information on which Clarius system is right for you.