Dr. Larry Istrail on Increasing Point-of-Care Ultrasound Awareness for Improved Patient Care
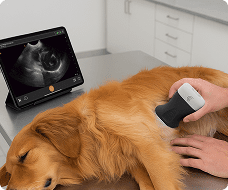
Dr. Larry Istrail, one of the foremost advocates of ultrasound, is a hospitalist in Northern Virginia, and treats patients who are admitted to the hospital for various non-surgical reasons, like pneumonia and heart attacks. He brought point-of-care ultrasound into his practice about six years ago, when he witnessed a colleague “doing a full body head-to-toe exam and getting the answers to the questions I had, which traditionally would take two to three days.”
“That really started me on this journey to see how incredible POCUS is, how it really gives you the superpower of looking inside people’s bodies and seeing their organs function in real time.”
Since then, Dr. Istrail has been on a journey to improve his ultrasound skills, and raise awareness around the benefits of POCUS to others around him.
On a recent episode of our Medical Imaging for All podcast, Larry shared what prompted him to write The POCUS Manifesto: Expanding the Limits of the Physical Exam with Point of Care Ultrasound, how point-of-care ultrasound awareness and education can increase, and what the future holds for POCUS.
The Origins of The POCUS Manifesto
It started with COVID, and the shifts around social distancing within the hospital. In addition to keeping themselves distanced from their patients, Larry noticed that clinicians stopped using a stethoscope. “They just decided to stop using that,” which he saw as “a tacit admission that maybe it wasn’t helping very much to begin with. But people were still using a lot of ultrasound,” which he saw could provide more information about the patient, especially for COVID.
This observation prompted Larry to write an article that appeared on STAT entitled “Will Covid-19 be the straw that breaks the stethoscope’s back?” in July 2020, which argues that “we are entering the era of point-of-care ultrasound.” But the response to the article was less than positive, with comments saying he was a technologist with no idea about medicine tradition, that medicine was going into the dumps, or fear that they would be taken care of by someone using ultrasound. “Like, crazy stuff when I’m trying to just argue for a technology that has better accuracy than a stethoscope,” he says.
But that was the eye opener that there was a general lack of understanding of what point-of-care ultrasound even was, or the benefits it could offer. So he decided to write a “short call-to-action manifesto to explain briefly the history and how it, in my opinion, is a transition from the auditory stethoscope exam into the visual exam. Just like radio to TV.” The POCUS Manifesto: Expanding the Limits of the Physical Exam with Point of Care Ultrasound was published in October 2021.
Solutions for Greater POCUS Adoption
What needs to change for an increase in POCUS adoption? It starts with a general increase in awareness, as ” older clinicians are more resistant in general. I haven’t had a lot of people who, in person, don’t understand or don’t appreciate it. It’s more they just haven’t experienced it.”
Then, after awareness comes education. Today, it’s a challenge for a busy clinician to learn it in their spare time, so “if it’s integrated into medical school, PA school, other school curriculum, then that is really what is needed.” This can happen more easily with today’s lowered price point on more portable devices.
Finally, there may need to be a rebranding of what POCUS is, as well as a reevaluation of the nature of the physical exam. As Larry explains, if you go to the doctor with a rash, they look at your rash, and inspect the skin. If you have pain in your wrist, a clinician would palpate it. “But what if you have chest pain? Right now, they just listen to it and then send you to get some testing. But why don’t you just look at it?” he asks. “A better name for appealing to people who don’t know what [POCUS] is would be ‘internal organ inspection,’ because that’s all you’re doing.” He argues that today, you don’t have to guess at the manifestations of an issue — you can simply look at it.
The Future of POCUS
One technology that can help close the education gap is artificial intelligence. As Larry explains, “to have an AI system that’s an assistant there for you to, say, move the probe left, rotate right, tilt up, or even to say, okay, this is a good quality image, or this is not a good quality image” would be a great benefit to clinicians.
There are also at-home and everyday possibilities for ultrasound as well. Larry cited a study where heart failure patients were given probes, taught how to use them, and were sent home to scan their own chest. “Then the images would be reviewed by someone.” Other at-home options could be scanning for pneumonia or even using ultrasound to check a fetal heartbeat, saving time, effort, and cost going to the hospital.