By many accounts, vision loss is the most feared disability in the general population. So, when a patient presents to the emergency department with acute vision loss, time is really of the essence and point of care ultrasound (POCUS) has become increasingly valuable in the diagnosis and management of ocular emergencies.
We recently hosted a popular one-hour webinar focused on ocular POCUS presented by renowned emergency physician and educator Dr. Tom Cook and moderated by Dr. Oron Frenkel, an emergency physician who practices in a busy academic teaching hospital. This free content-rich webinar is available to watch on-demand now: Ocular POCUS: Diagnosing, Traumatic Eye Injuries and Avoiding Vision Loss. Read on for highlights.
Key Takeaways from Dr. Tom Cook’s Ocular POCUS Webinar
I don’t think most people even think of using ultrasound to look at an eyeball but it is basically a bag of water, so it turns out to be a wonderful tool for evaluating ocular pathology,” says Dr. Cook at the start of the webinar.
If you look at different studies, about 3% of patients who present to emergency departments have some kind of visual complaint. And if you think one in 33 patients have this a complaint, this is actually pretty prevalent as it comes into the emergency department. So, we really need to be able to manage these patients.”
Why Ocular POCUS Matters
- High Prevalence of Visual Complaints: 3% of ED patients present with eye issues, making it crucial for EPs to have effective diagnostic tools.
- Limitations of Traditional Exams: Fundoscopic exams are often challenging due to poor physician skill, patient cooperation, and trauma-related swelling.
- Time-Sensitive Diagnoses: Acute vision loss can be caused by conditions like vitreous hemorrhage, retinal detachment, and globe rupture, requiring rapid assessment and management.
POCUS in Ocular Emergencies: Advantages
- Improved Diagnostic Accuracy: POCUS significantly enhances the ability to detect retinal detachment, vitreous hemorrhage, lens dislocation, and other critical conditions.
- Ease of Use: The technique is simple, requiring only an eyeball and ultrasound gel, making it accessible to EPs of all skill levels.
- Rapid Assessment: Exams can be completed in seconds, expediting patient care and disposition.
- Patient Comfort: Non-invasive and painless compared to traditional eye exams.
Key Ocular Pathologies and POCUS Findings
- Vitreous Hemorrhage: Presents with floaters, flashes, and cloudy vision. POCUS shows a “big blob” or low-attenuation hyperechoic material in the posterior segment.
- Retinal Detachment: Presents with flashes, floaters, and a “curtain” of vision loss. POCUS shows the retina detached from the choroid, with the key distinction being “mac on” (macula attached, urgent) vs. “mac off” (macula detached, less urgent).
- Posterior Vitreous Detachment: Common in older adults, presents with floaters and flashes. POCUS may show a subtle line across the posterior segment, often requiring increased gain for visualization.
- Lens Dislocation: Often caused by trauma, presents with significantly decreased visual acuity. POCUS shows the lens out of place, sometimes with visible zonular fibers.
- Globe Rupture: Typically due to trauma, presents with severe vision loss and facial trauma. POCUS may show a “flat tire sign” or disruption of the normal ocular anatomy.
- Retrobulbar Hematoma: Often associated with trauma and restricted eye movement. POCUS shows hypoechoic areas in the retrobulbar space, indicating bleeding.
- Increased Intracranial Pressure: Can present with headaches, blurred vision, and papilledema. POCUS shows a “poofing out” of the optic disc and an enlarged optic nerve sheath diameter (>5mm).
Pearls and Pointers
- Increase the gain when subtle findings are suspected, especially with vitreous hemorrhage and posterior vitreous detachment.
- Involve ophthalmology early, particularly in cases of retinal detachment and other vision-threatening conditions.
- Don’t hesitate to use POCUS even if globe rupture is suspected; gentle technique with ample gel minimizes risk.
- Consider optic nerve sheath diameter as an adjunct in assessing for increased intracranial pressure.
VIDEO: Ocular Ultrasound Demonstration with Clarius PAL
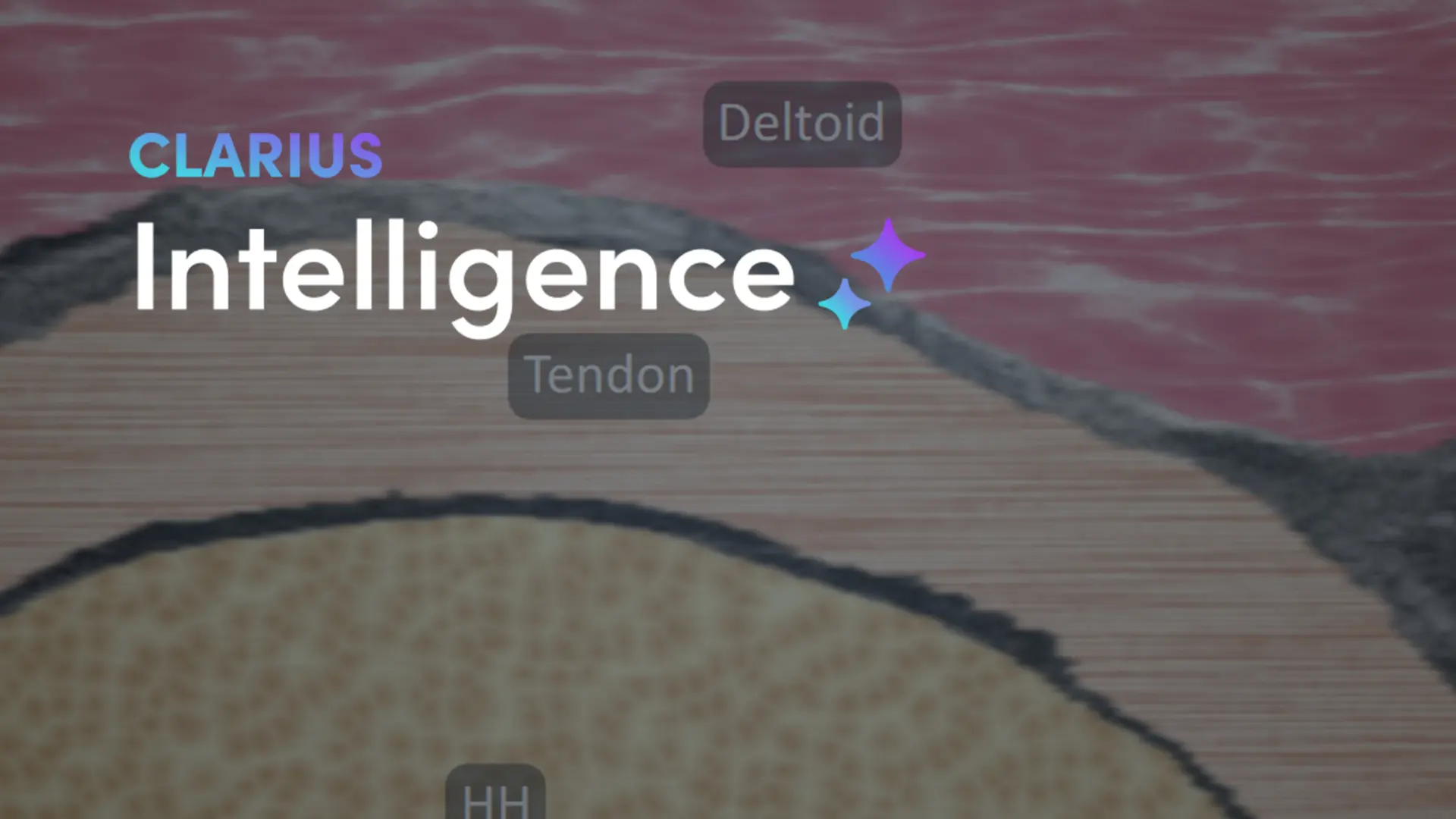
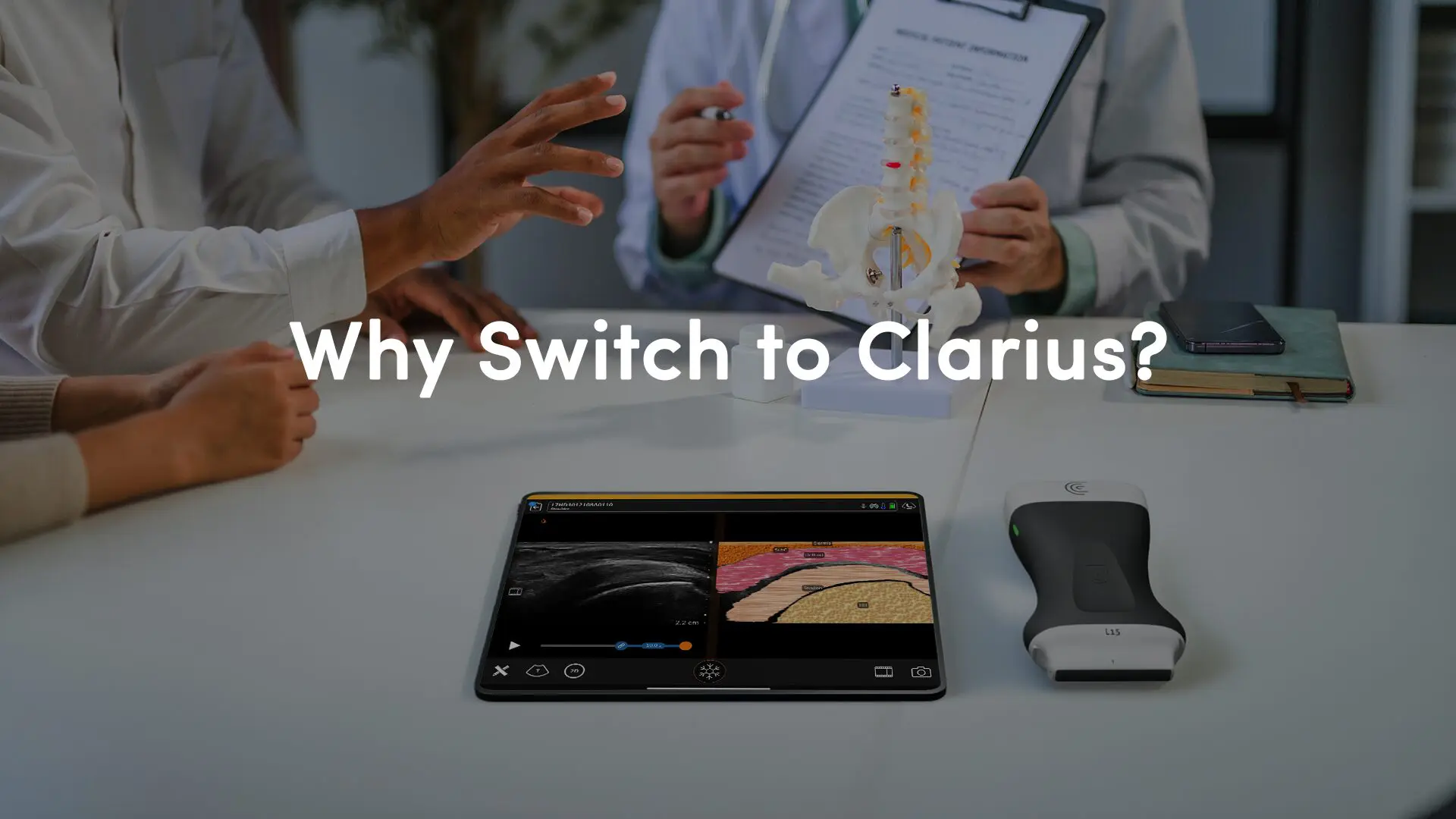
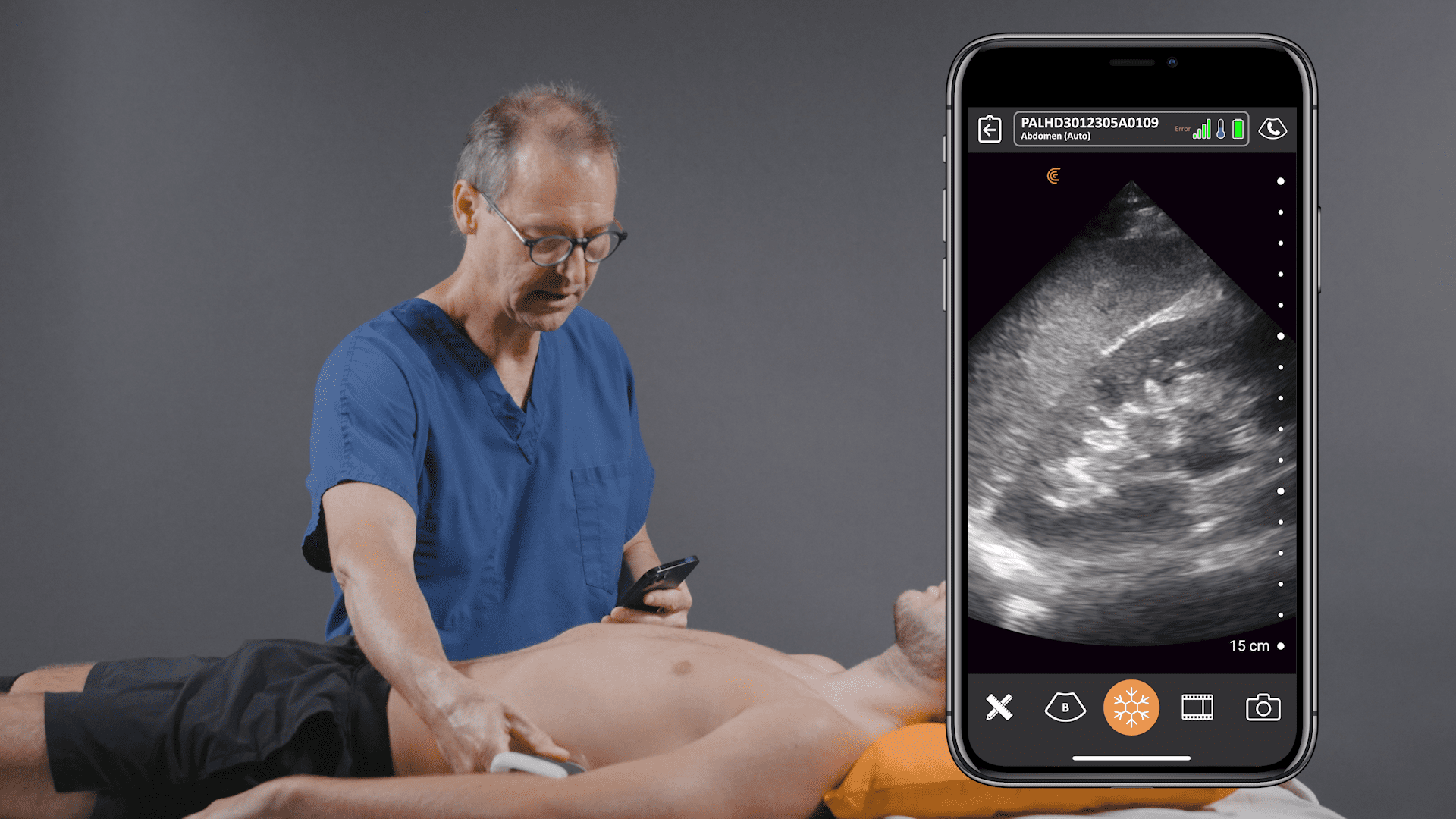
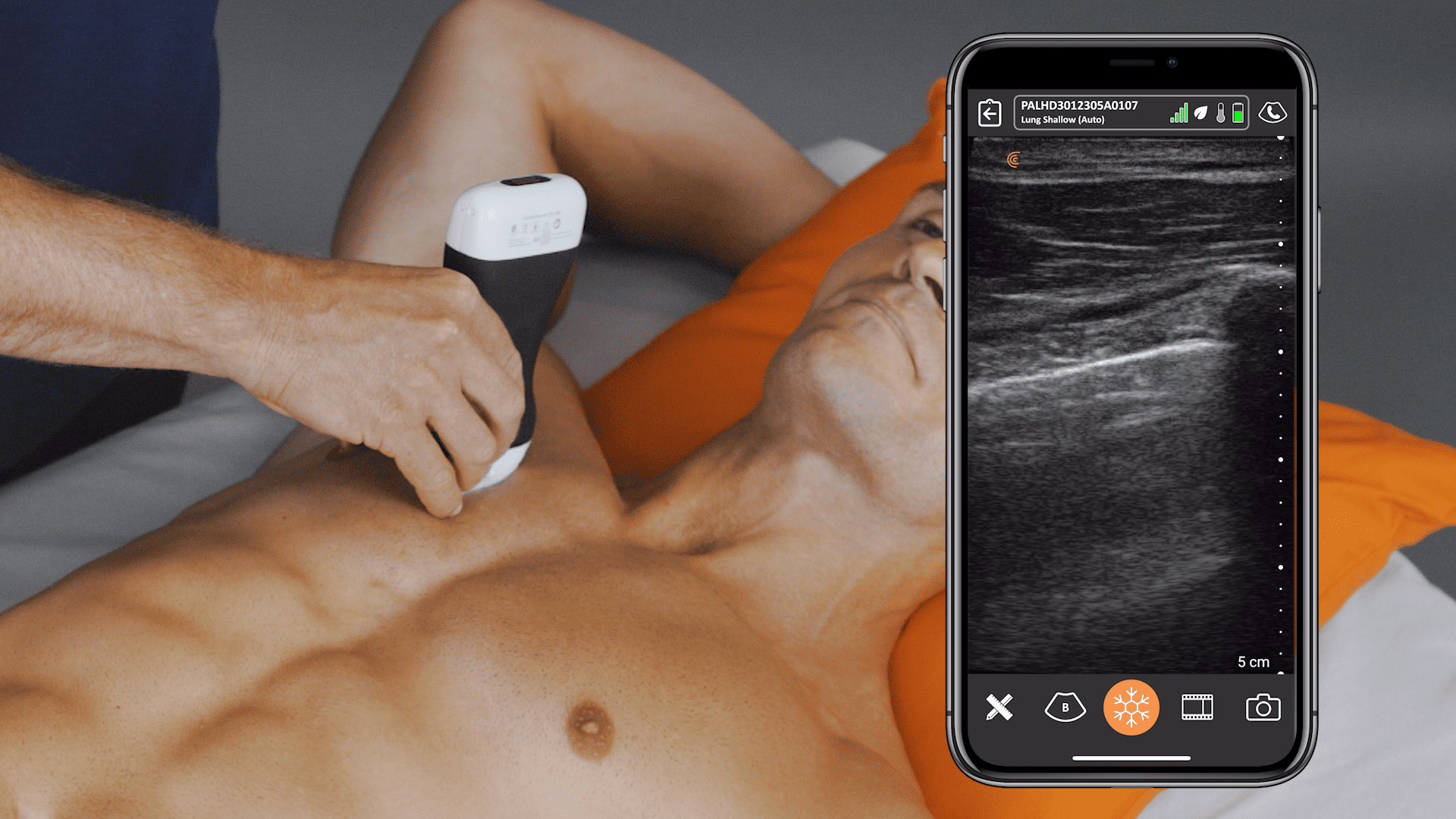
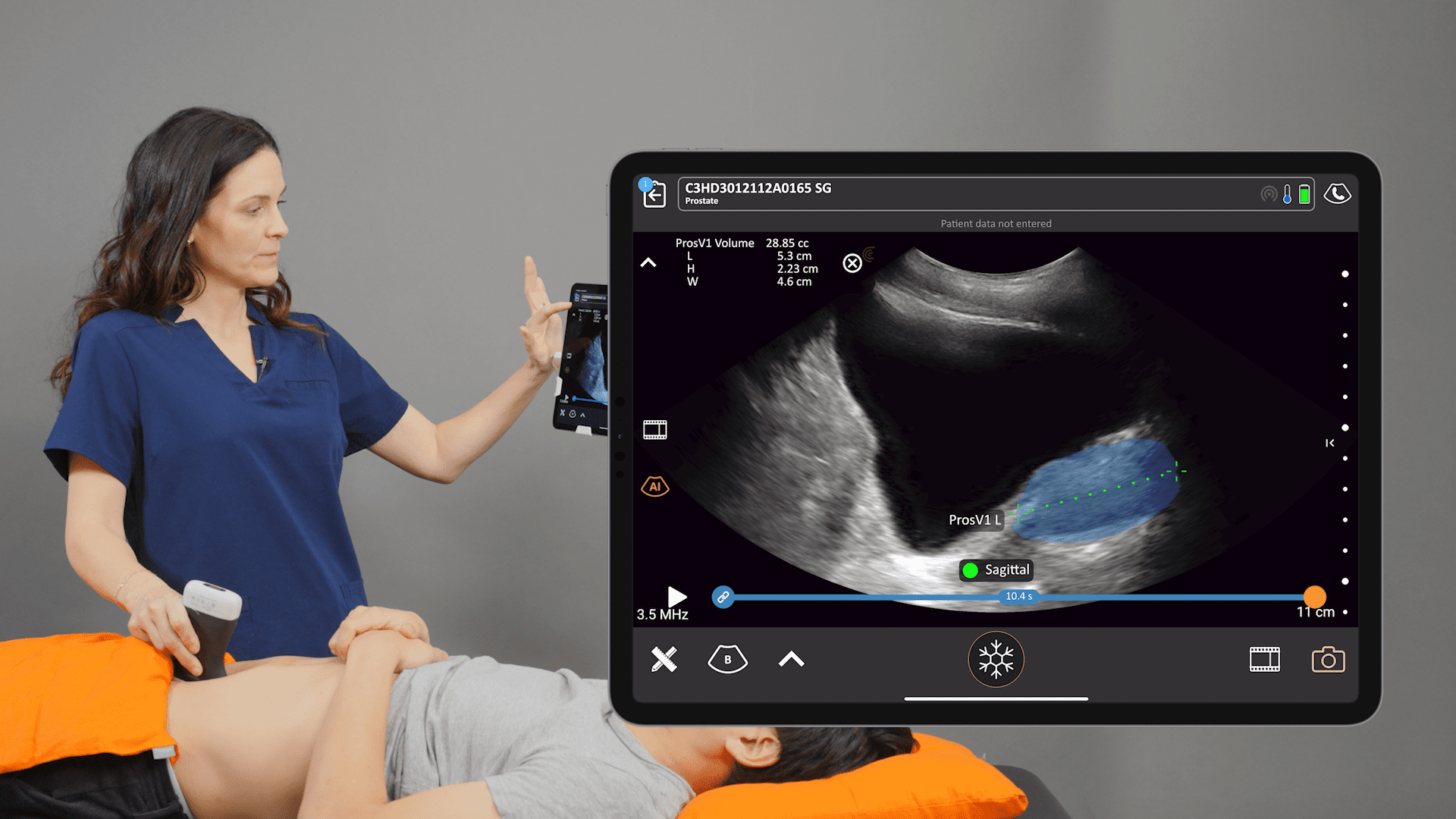
Watch this 2-minute video to see sonographer Shelley Guenther demonstrate how to scan for a rapid assessment for retinal detachment or vitreous hemorrhage using the Clarius PAL HD3 dual-array wireless handheld ultrasound scanner. Our newest scanner, Clarius PAL is designed to provide superior image quality for whole-body imaging.
Learn more about Clarius for emergency medicine and primary care. Contact us for a personal virtual demo if you’d like to discuss which Clarius scanner is right for your practice.