A relatively simple and risk-free procedure, the Pectoral Nerve (PECs) block is widely used to control post-operative pain, particularly following breast surgeries.
A 2020 study published by the Department of anesthesiology at Stony Brook University Health Science Center analyzed 19 randomized control trials and concluded: “When compared to general anesthesia with systemic opioids, PECs block was associated with significantly better perioperative pain control.”
When Dr. Gregory Hickman, the medical director and anesthesia director at an orthopedic surgery center, noticed patients suffering from severe pain in the axillary region, he discovered another application for a PECs block.
Preoperatively, we were doing interscalene blocks and catheters. So, they had no shoulder pain but they were really struggling with axillary pain,” explains Dr. Hickman. “One day I decided to try a PEC 1 and a PEC 2 block to see if they would take care of the axillary pain. Well, I did the PEC 1 and boom: the pain was gone! I didn’t even proceed to do the PEC 2 part of the block because the patient was doing fine.”
Dr. Hickman’s team research into the technique found physicians at Wake Forest University using the PEC 1 and 2 block for biceps tenodesis. “Their theory was the spread from the PEC 1 goes laterally to the intercostal brachial nerve, which we know as T2 and T3. Mostly T2 comes into the axillary region and affects the skin and superficial areas, which explains the effectiveness of this block,” he explains.
Read on for Dr. Hickman’s master tips on performing PECs injections.
Instructions for an Ultrasound-Guided PECs Block Using Ultrasound Guidance
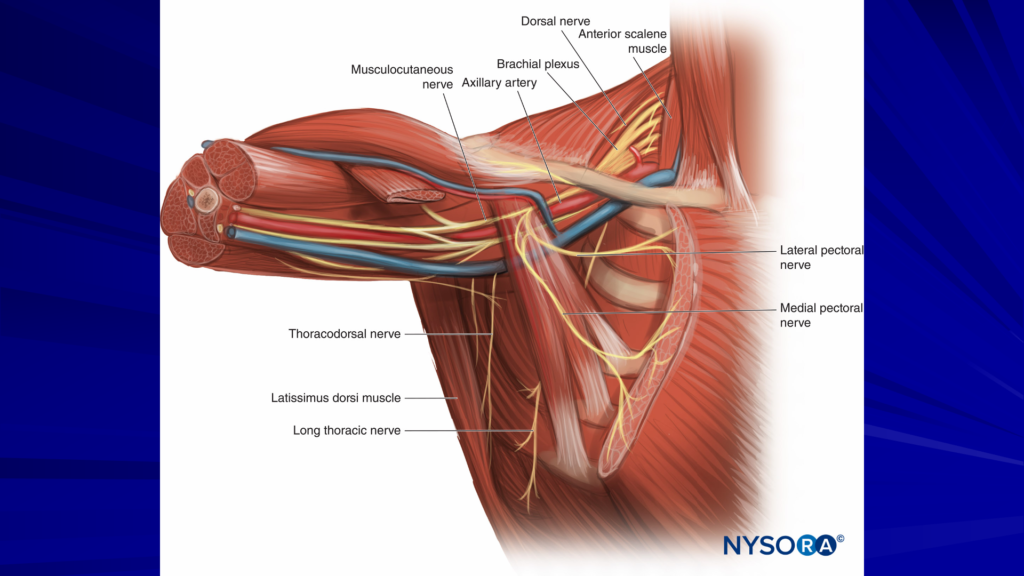
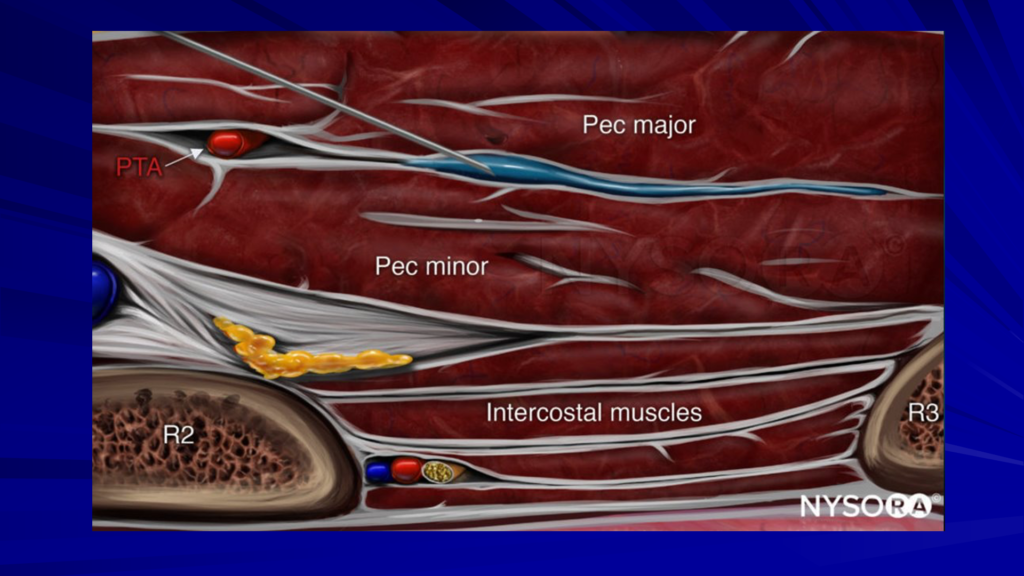
„The PEC 1 is an injection between the pec major and the pec minor, and it blocks the medial and lateral pectoral nerves. The medial and lateral pectoral nerves are branches of the medial and lateral cords. We’re inject between those two nerves.
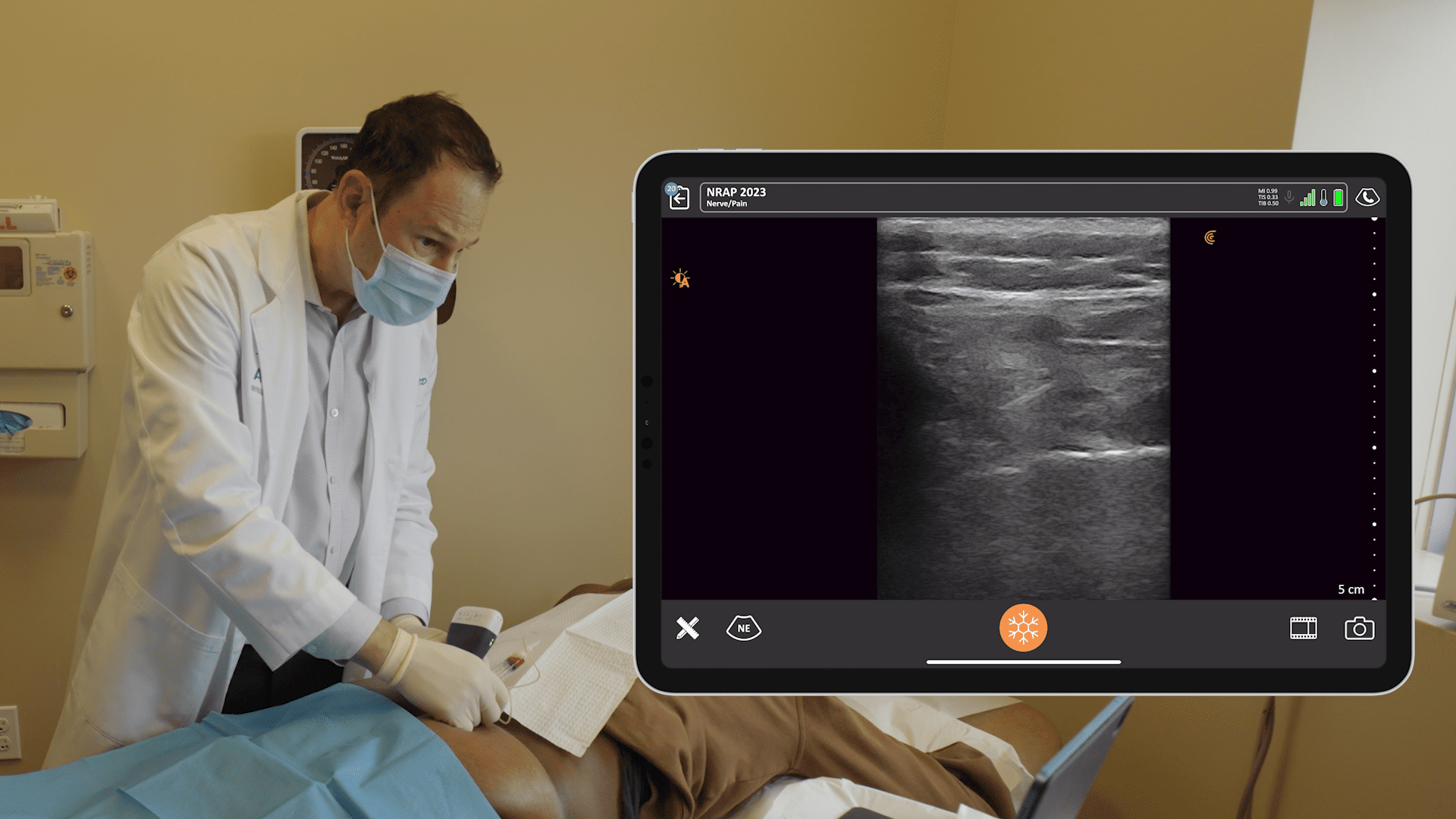
This is a really simple block. We just get as lateral as we can between the pec major and pec minor and we inject 10 cc of 0.25% bupivacaine. Ultrasound makes the procedure much easier to do. So, pec major, pec minor, just get in this plane, come out a little lateral, and that’s what we’re looking for.
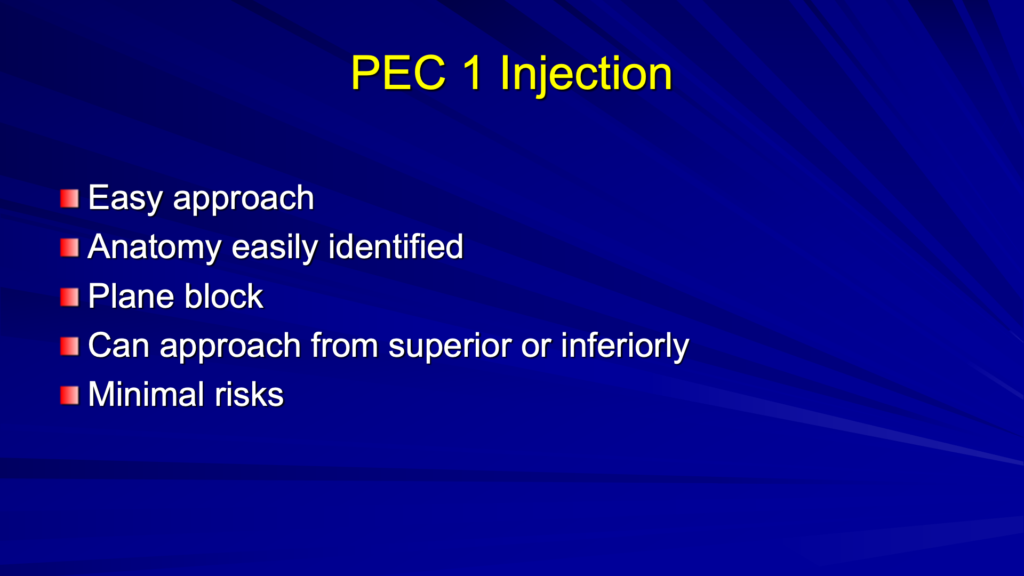
It’s an easy approach. The anatomy is very easily identified on ultrasound. The pec muscles are pretty easy to see.
This is an interesting block because you can approach it superiorly or inferiorly to the probe. I prefer to go superiorly most of the time. Sometimes I’ll come inferiorly depending on what I see. There’s minimal risk so you can watch what you’re doing and put it in this plane using ultrasound.
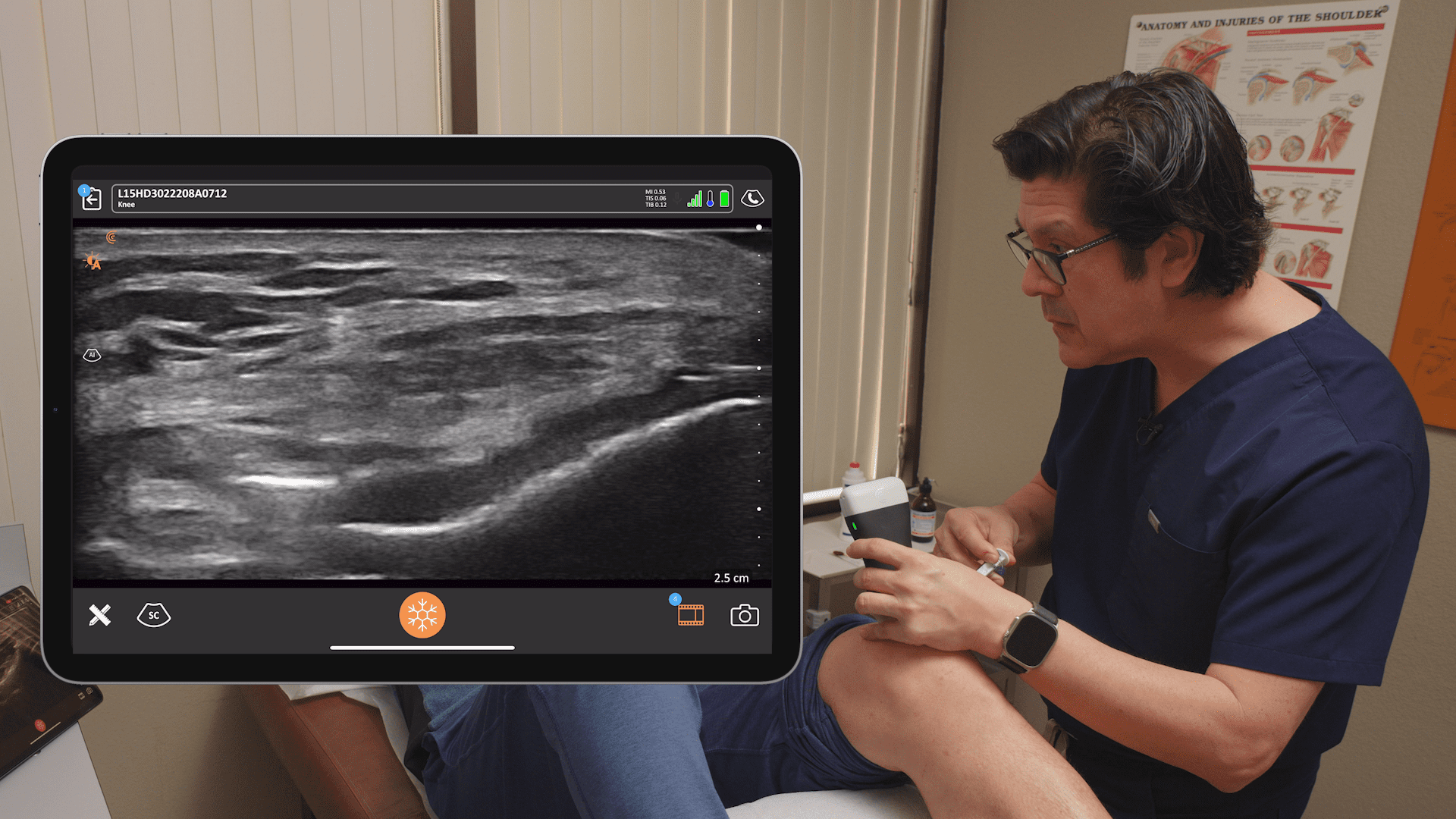
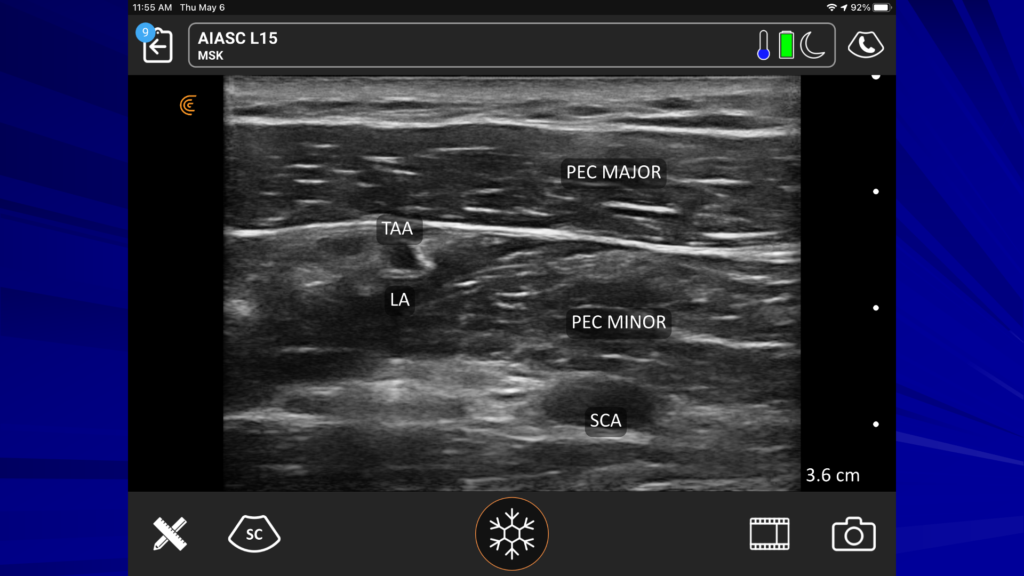
In the ultrasound image above, you see the pec major and the pec minor. If you see the subclavian artery, down under the pec minor, you know you can see the pec major and the pec minor very well. I shoot for the thoracoacromial artery. I drop a little local around that area and also in the plane between the two muscles.
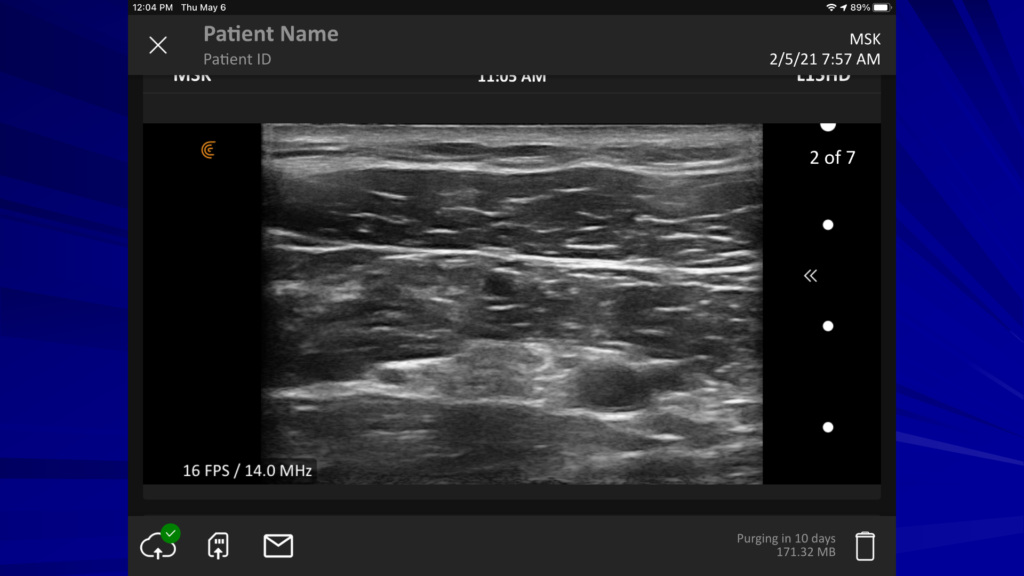
Here’s the same image without the labels so you can identify the structures for yourself.

This view is to show you the clavicle on the left. I got up a little higher, a little more cephalic.
Video Demonstration of the PEC 1 Block
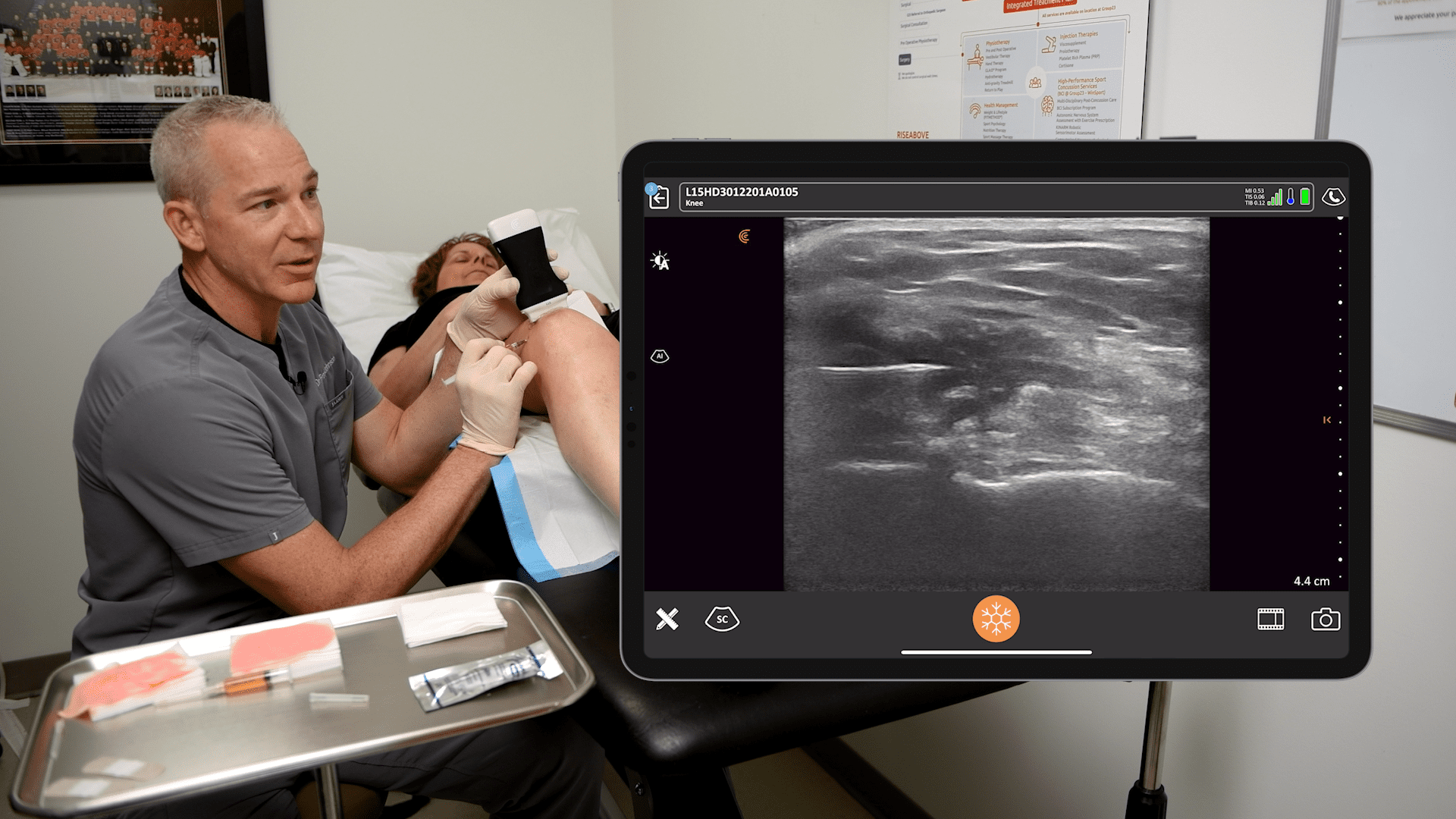
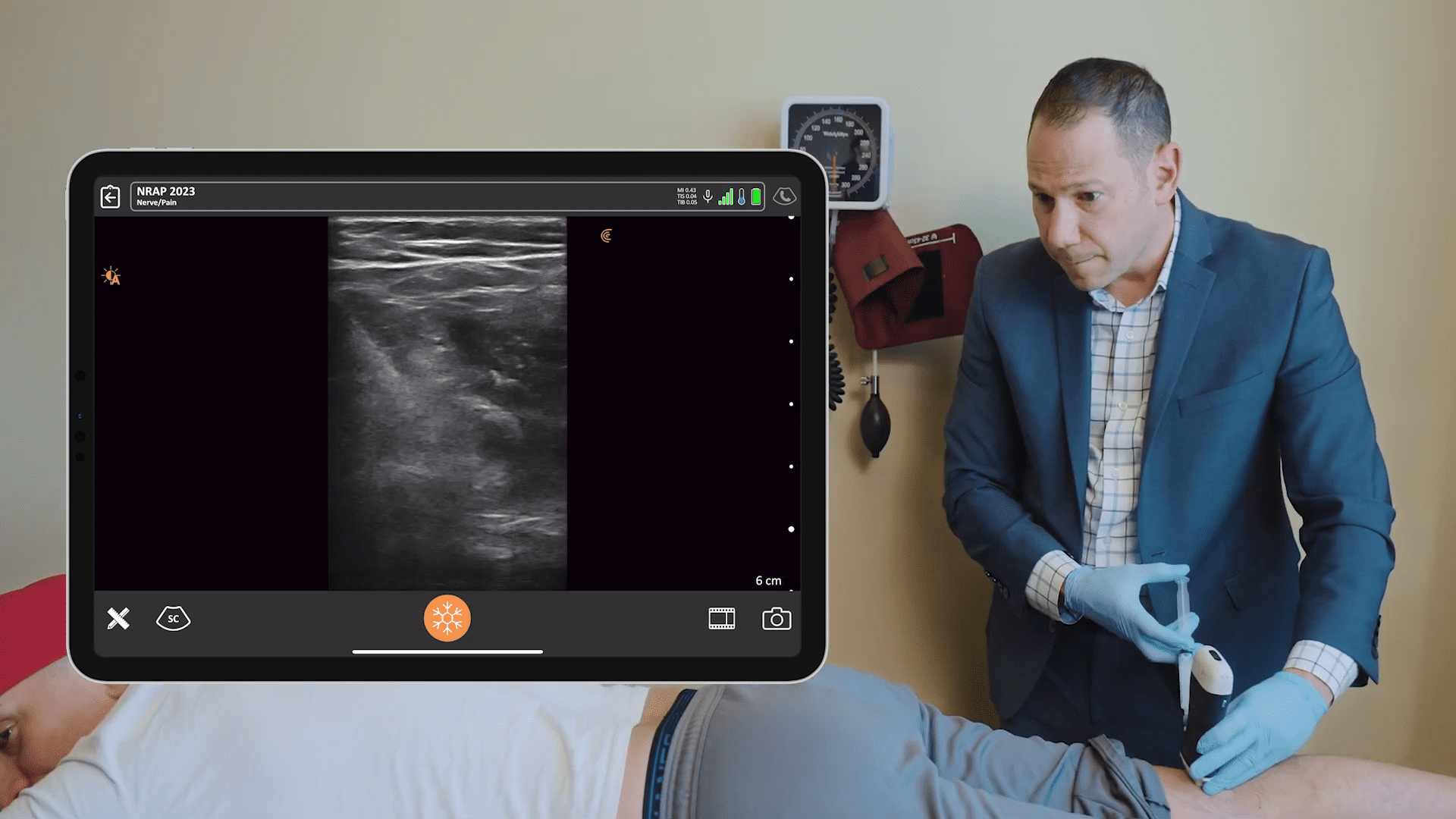
In this video, you see I’ve got my iPad placed on the patient’s abdomen. I’m coming in from an inferior approach. You can see a nice big pec major. It’s really easy. There are no cords, no cables coming off so we can take a nice approach and get a nice view. You have your line of sight with your needle and your iPad lined up so you can see everything as you’re approaching. You can control the ergonomics by placing the iPad wherever you want it. I use an iPad mini, which works great.
Watch our needle coming in and you see the pec major, which is a little deep. You’ll see the subclavian artery as the space opens up between the two muscles. You can see how easy it is just to move that probe around and keep a good view.
It’s pretty great to have the screen so close for the perfect shot. It’s really easy to add depth to show that subclavian artery. I just touch the screen. It’s so easy to change my view and to change the gain by just swiping to the right and left on the screen.
I’m showing where the biceps tenodesis incision is going to be right there in the axilla. We can watch the local spread to get to the intercostal brachial nerve.“
Watch a Complimentary Webinar About Ultrasound-Guided Regional Anesthesia
Dr. Greg Hickman is currently the medical director and anesthesia director at the Andrews Institute Ambulatory Surgery Center in Florida. Over the past 30 years, he has perfected the art and science of ultrasound-guided injections to deliver maximum pain relief. He joined Clarius for a one-hour webinar to share his master tips for performing three ultrasound-guided injections in the webinar „The Mobile RA: Using Handheld Ultrasound to Guide PEC and Supraclavicular Blocks Plus Intra-Articular Injections.“ Watch the webinar recording of the full session at your convenience.
Interested in Using Clarius Ultrasound for Your Regional Anesthesia Practice?
During the video demonstration, Dr. Hickman used the Clarius L15 HD, a high-frequency linear ultrasound scanner with a maximum depth of 7 cm.
Wireless and pocket-sized, Clarius scanners deliver the high-definition imaging and power you expect from a traditional ultrasound system in a highly affordable ultra-mobile scanner. Visit our regional anesthesia specialty page to learn more about Clarius. Or book a demo for information on which Clarius system is right for you.