A trail-blazing orthopaedic surgeon, Dr. Alan Hirahara has been using ultrasound for procedure guidance for more than 10 years. With the emergence of new treatment options including orthobiologics, like PRP, he believes ultrasound guidance is more important than ever.
Corticosteroids have a lot of risks and I’m appalled that I don’t hear doctors talking to their patients about it because we know these risks exist,” says Dr. Hirahara. “They soften and damage cartilage and weaken or rupture tendons. That’s why you can never put a corticosteroid into a tendon, into an area where you’re going to damage the structure, and actually cause it to have an increased risk of rupture and tear. Ultrasound helps us ensure we place the injection in the right place.”
Dr. Hirahara recently presented a one-hour webinar on using ultrasound for accurate and painless MSK injections. Watch his webinar or read on for some highlights including a video case study and his thoughts on new treatment options.
The Risks of Corticosteroids
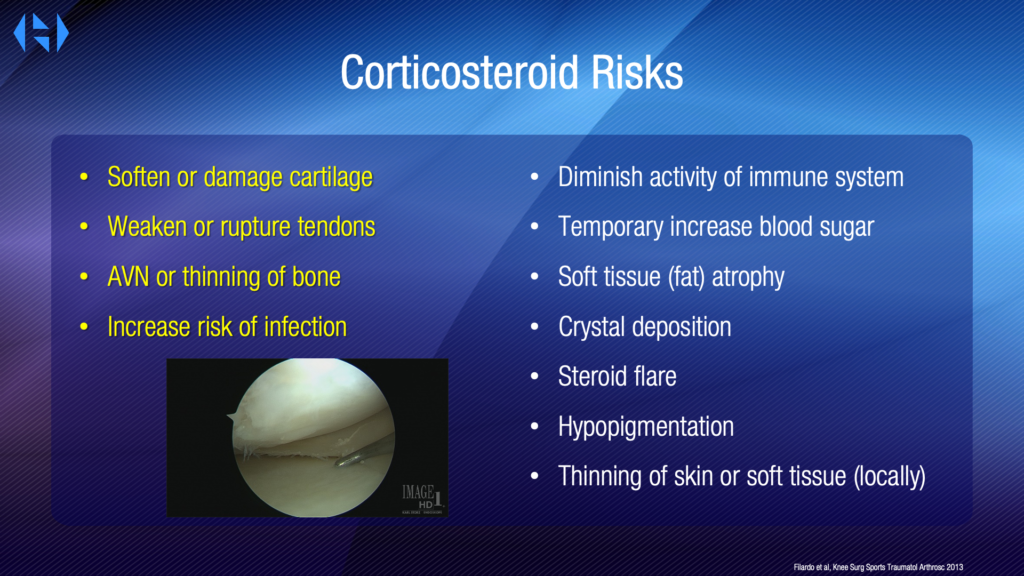
“We never want to put corticosteroid into a tendon as it softens and damages cartilage, weakens or ruptures tendons.
There’s also increased risk of AVN, thinning of the bone, increased risk of infection, which can diminish the activity of the immune system, temporary increase blood sugar with diabetics, soft tissue fat atrophy, crystal deposition, steroid flare, hypopigmentation, and thinning of the skin. All this can occur and will even affect us surgically.
We now have numerous studies that show a negative effect of preoperative cortisone on rotator cuff outcome with increased risk of revision. It can occur with just one injection. It increases the time to surgery because you want to make sure there is no risk that the surgery will fail due to a previous cortisone treatment.
PRP Is No Longer Experimental
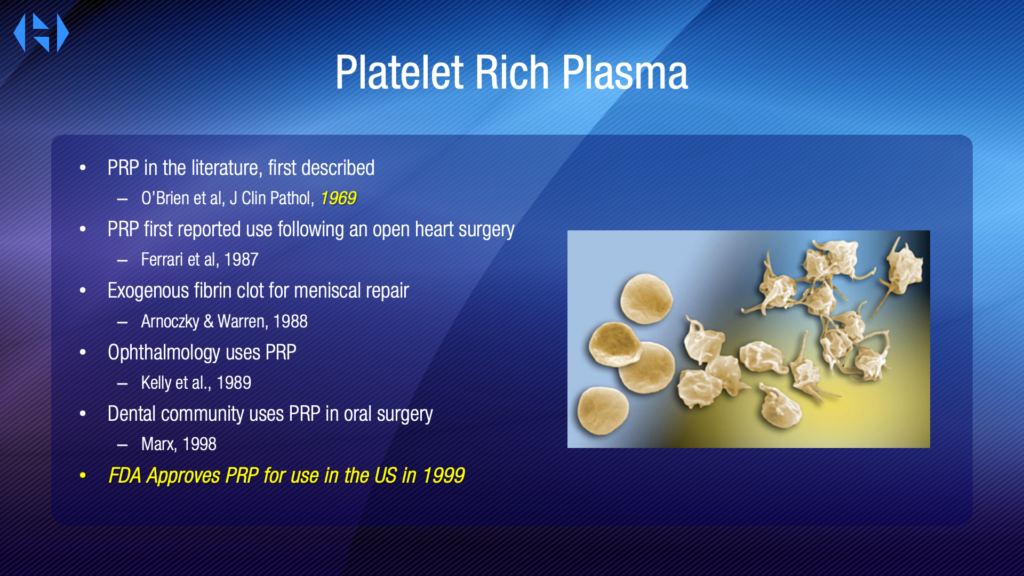
PRP, which was first described in the literature in 1969, has become very prominent in the past decade or two. More studies started to emerge in the 80’s and it was FDA approved for use in 1999. So why in 2021, do we still consider PRP experimental?
There’s plenty of basic science research that has been showing that it augments proliferation of tenocytes, osteoblast myocytes, diminishes inflammation, diminishes pain, augments HA secretion, and augments stem cell migration proliferation. There is a ton of data now that shows that this is what happens, and really, we shouldn’t be surprised. Because how do you think our body heals? The body doesn’t heal by fairy dust; our body has platelets as the first step in our process from injury to healing. It doesn’t do all the work; it’s a whole process. And our goal is to understand the process and intervene with those products, with those things that our body has to use in the treatment of disease and injury.
Making the proper diagnosis, understanding what’s wrong, and then applying that biologic in the manner it’s needed to the problem will help us get a better outcome.
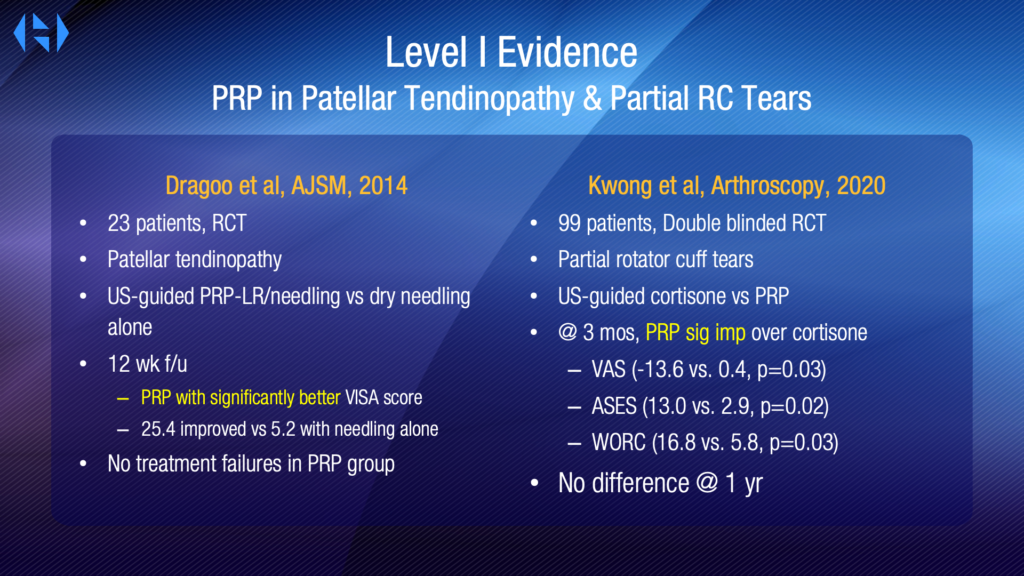
There is level one evidence that PRP is very effective in DJD, superior to HA, superior to placebo, and superior to cortisone. Level one evidence that PRP is better in patellar tendinopathy and partial rotator cuff tears. PRP promotes stem cell migration and proliferation because that’s its job. Platelets, with their release of alpha granules, promote proliferation and migration of the stem cells, which do the work.
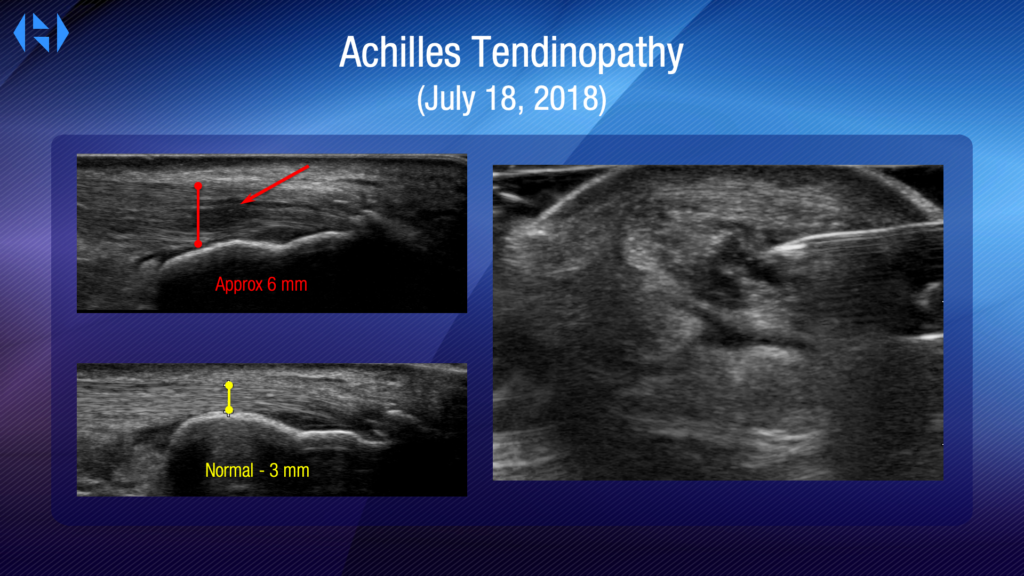
Treating Achilles Tendinopathy with an Ultrasound Guided PRP Injection
Here’s an example of an achilles tendinopathy. And this is near and dear to my heart because this is my achilles. My achilles in 2018 was in really bad shape. And you can see the hypoechoic area in the tendon. You can see that my tendon was six millimeters wide. Normal thickness is three millimeters.
Here is my Achilles six weeks after injecting PRP into the defect. There’s a big difference. Was it normal? It still wasn’t normal. 3.7 is a big difference from 6; and the pain level was significantly different.
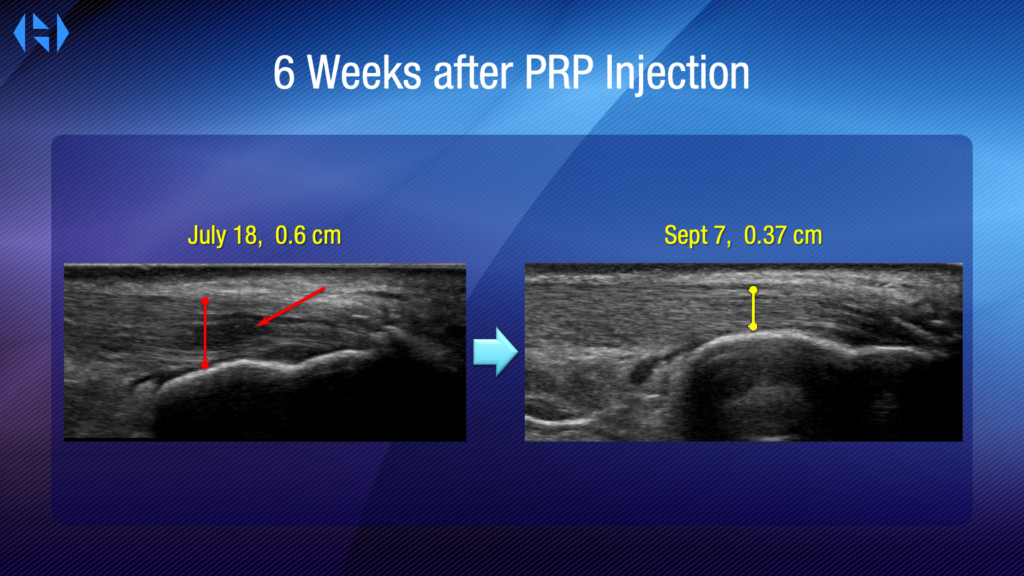
I can tell you that today, three years later, I have no pain. My ultrasound looks absolutely normal as if nothing had ever happened. The point is that I know as a client that these treatments do work, and using ultrasound is important to get it to the exact spot.
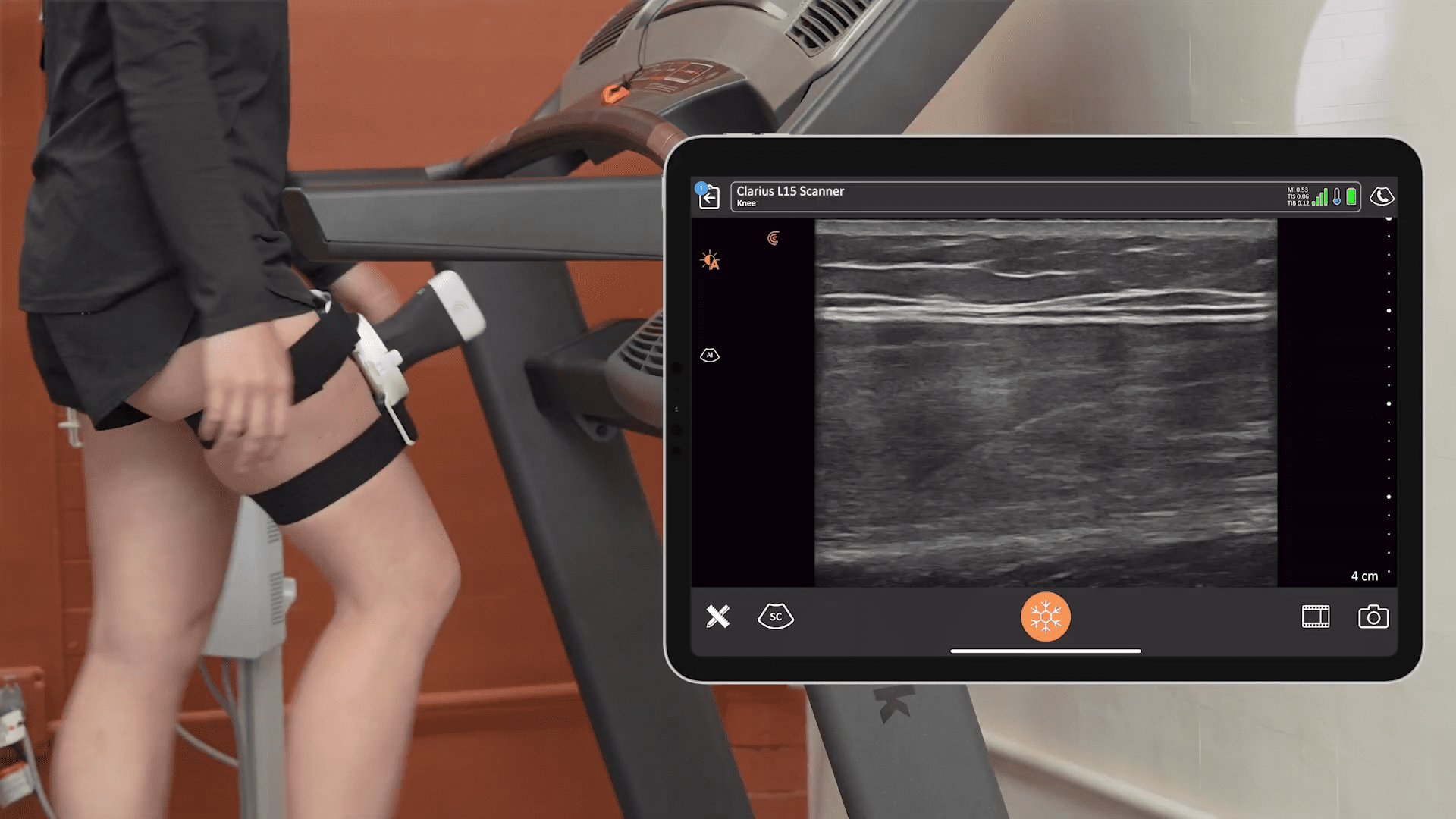
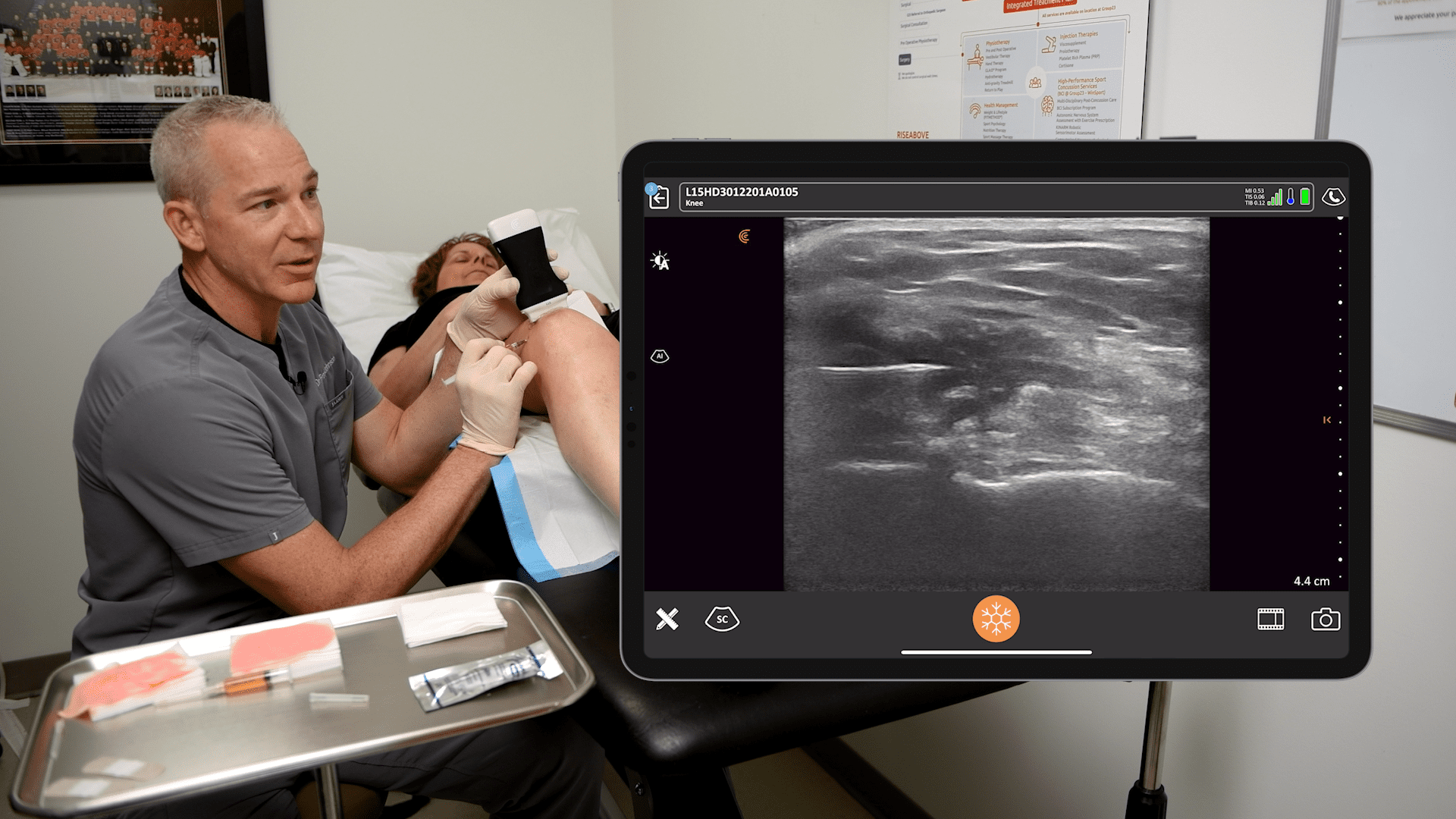
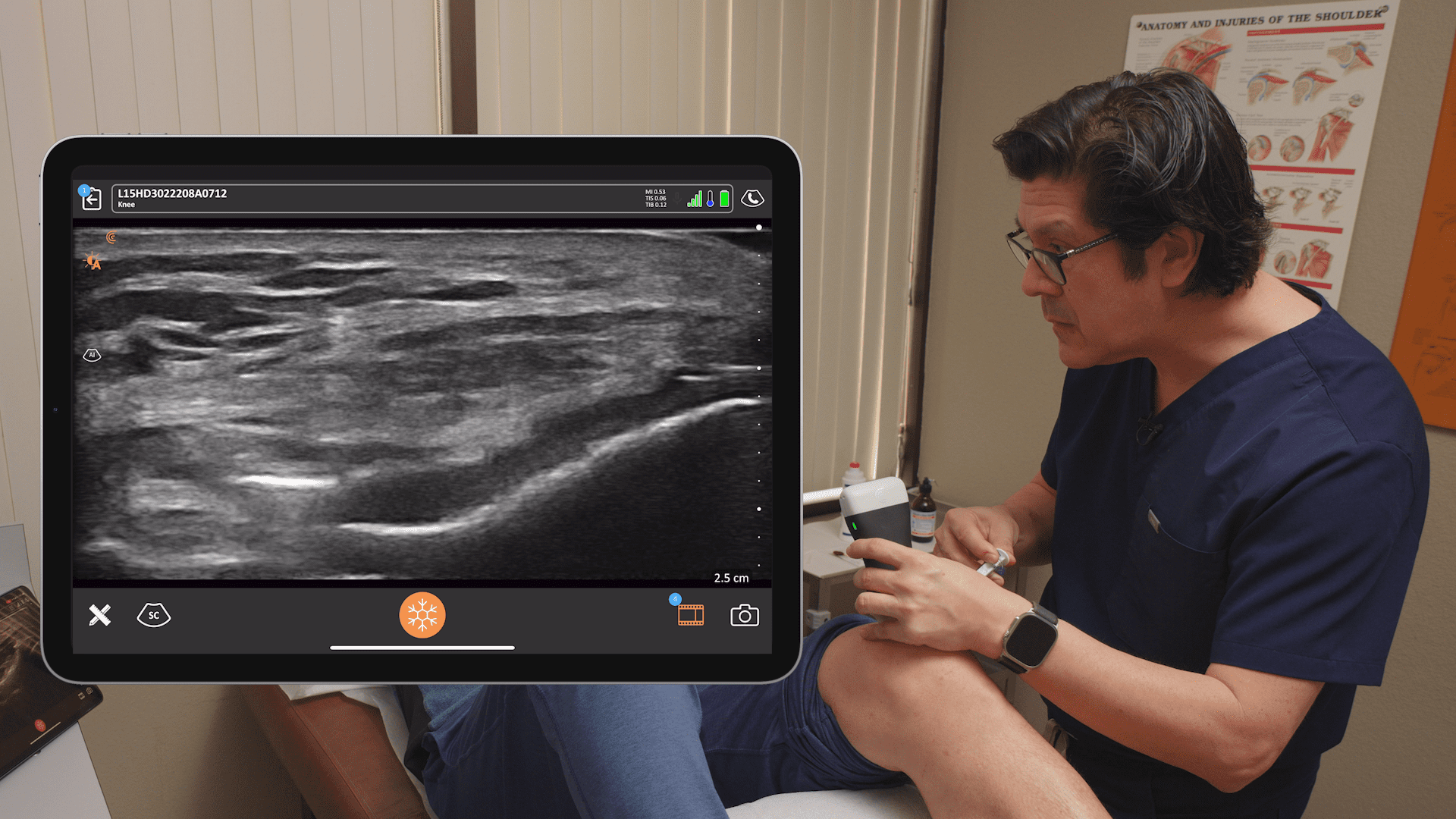
Video: An Intra-Tendinous PRP Injection Using the Clarius L15 to Bring Pain Relief
Watch Dr. Hirahara perform an intra-tendinous PRP injection using ultrasound guidance to bring pain relief to a patient suffering from lateral epicondylitis.
About Dr. Hirahara
Dr. Hirahara is board certified in both orthopaedic surgery and orthopaedic sports medicine in both the United States and Canada. He was recently appointed to the NCAA committee on Competitive Safeguards and Medical Aspects of Sports and is currently involved with the Health and Safety Committee for the Big Sky conference. He’s the medical director and team physician for California State University, Sacramento athletics and head team physician for the Sacramento River Cats and a triple A affiliate of the San Francisco Giants.
Handheld Ultrasound for Orthopedic Surgery
Dr. Hirahara uses the Clarius L15 for his practice. Visit our orthopaedic surgery specialty page or contact us for to learn more about adding handheld ultrasound to your practice.