By Daniel J. Kim, MD FRCPC
As the COVID-19 pandemic has evolved, it is clear that cardiovascular complications are common, including pathology like myocarditis, acute coronary syndrome (ACS), heart failure, cardiogenic shock, and venous thromboembolism (VTE).1 Echocardiography is an important tool in the assessment and monitoring of these complications.
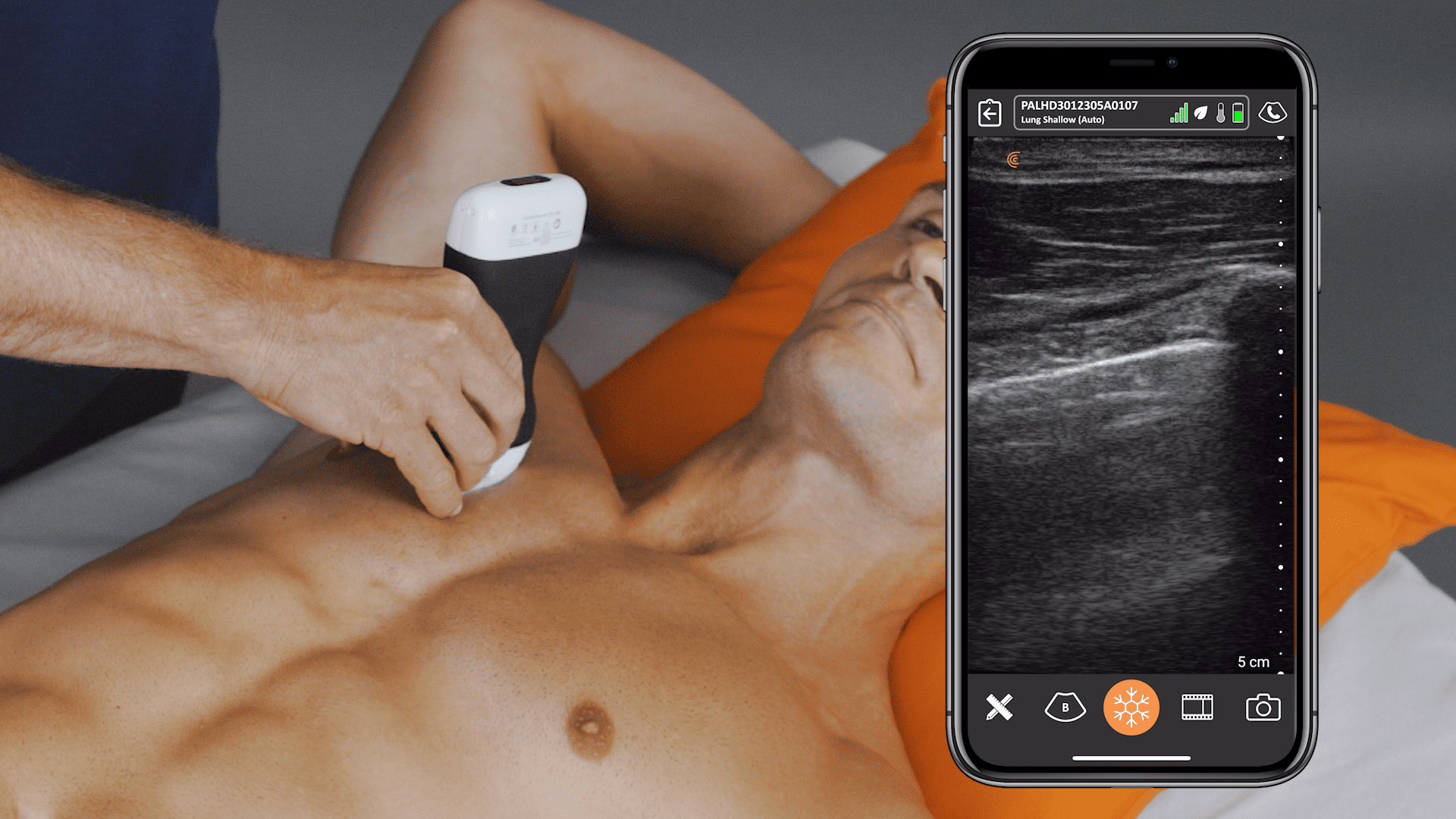
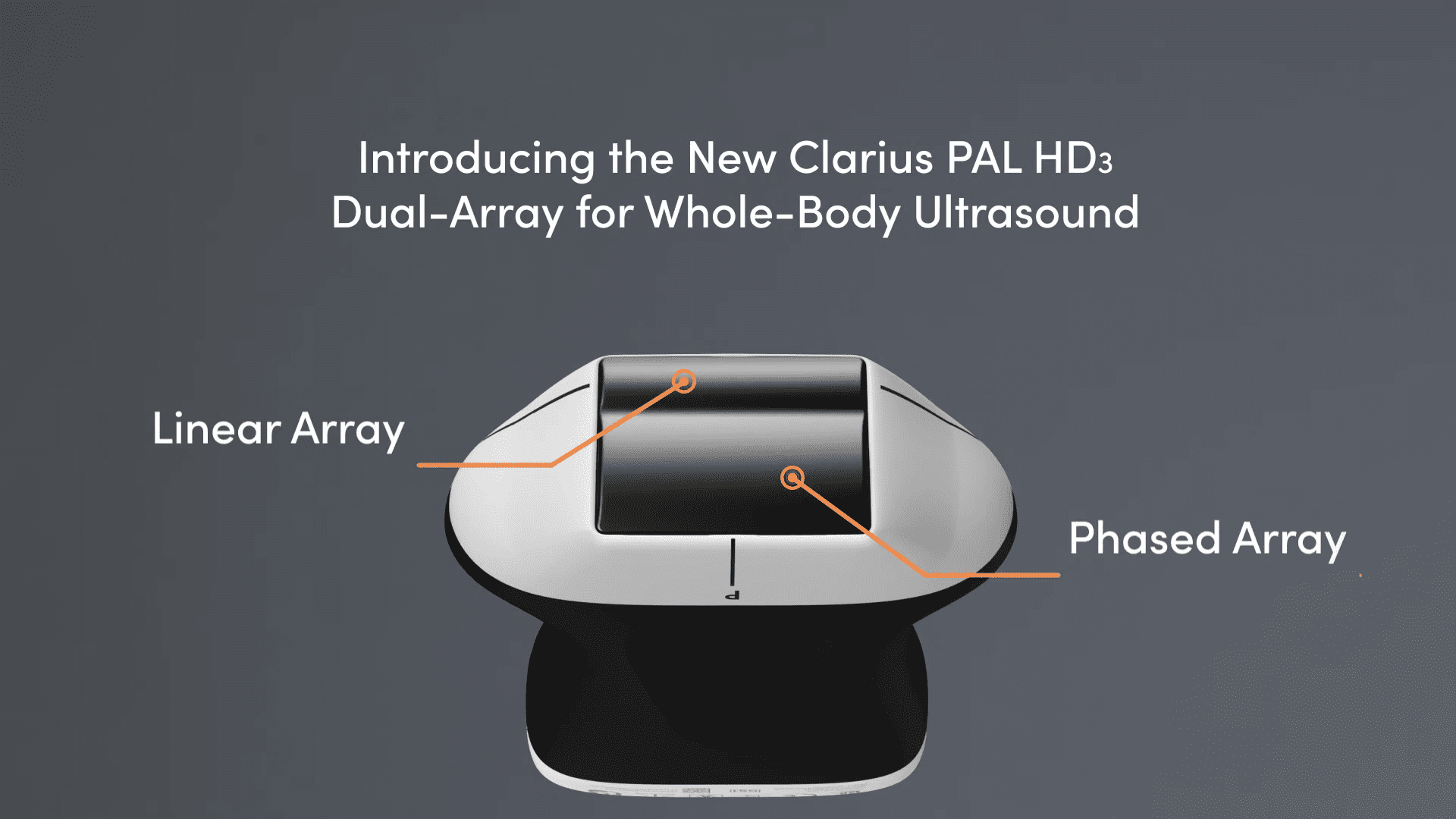
In fact, the American Society of Echocardiography (ASE) published a statement endorsing the use of point of care ultrasound (POCUS): “the rapid, bedside assessment of the heart, chest, and vessels by POCUS has propelled this tool to the frontlines of the fight against the COVID-19 pandemic.”2
The European Association of Cardiovascular Imaging (EACVI) published recommendations advocating for all echocardiograms to start as a focused scan assessing the left ventricle (LV), the right ventricle (RV), and the pericardium.3 This is an excellent framework to use at the point of care for the clinician taking care of sick COVID-19 patients in the emergency department, the inpatient ward, or the intensive care unit.
Left Ventricle
Cardiac involvement in patients with COVID-19 is high. Guo et al reported a 28% rate of myocardial injury in 187 patients with COVID-19, defined as a positive troponin. Patients with a positive troponin had a mortality rate of 60% compared to 9% in patients without a troponin elevation.4 Similarly, Shi et al found a 20% rate of myocardial injury in 416 patients with COVID-19. Again, mortality was much higher in the group with an elevated troponin (51%) compared to the group without a troponin elevation (5%).5 The exact mechanism behind myocardial injury isn’t known, but various processes may be involved, including angiotensin-converting enzyme 2 (ACE2), cytokine storm, direct viral damage, and hypoxia.
The LV is a good place to start, especially in the setting of myocarditis and cardiomyopathy. Case reports have described LV systolic dysfunction,6 takotsubo cardiomyopathy,7 and wall motion abnormalities.8
Eyeball assessment of LV systolic function is adequate, as the priority is to identify a major problem. This should be assessed by examining 3 aspects of LV function: endocardial excursion, myocardial thickening, and movement of the mitral valve.
- Endocardial excursion: This is the movement of the walls of the LV into the chamber. The endocardium should move symmetrically toward the center of the LV during systole.
- Myocardial thickening: This refers to the increase in the thickness of the myocardium by about 40% in all LV segments during systole. This should occur symmetrically.
- Mitral valve movement: In a heart with normal LV systolic function, the anterior leaflet of the mitral valve should come within 1 cm of the septum in early diastole.
New global LV systolic dysfunction is suggestive of myocarditis, while regional wall motion abnormalities are more suggestive of ACS.

Right Ventricle
Another COVID-19 issue is the high rates of venous thromboembolism (VTE) in patients with severe disease. Cui et al reported a 25% incidence of VTE in 81 ICU patients with COVID-19.9 Klok et al described their experience in the Netherlands with 184 ICU patients with COVID-19, and they identified a 27% incidence of VTE. A majority of these cases were pulmonary embolisms (PEs).10
Although echocardiography is poorly sensitive for PE, it has reasonably high specificity. Echocardiographic signs of PE reflect right heart strain and dysfunction.


Keep in mind that some patients develop right heart dysfunction and pulmonary hypertension due to COVID-19, acute respiratory distress syndrome (ARDS), and mechanical ventilation, even in the absence of PE. Echocardiographic findings of right heart dysfunction should be interpreted in the context of the clinical scenario and other investigations like the d-dimer or assessment of the leg veins for deep vein thrombosis.
Newer evidence shows that echocardiographic signs of right heart dysfunction are associated with mortality. Li et al assessed 120 consecutive patients with COVID-19 and found that more advanced RV measurements like RV longitudinal strain, RV fractional area change, and tricuspid annular plane systolic excursion (TAPSE) were independent predictors of higher mortality.11 Argulian et al reported a 31% incidence of RV dilation in 105 patients with COVID-19. Mortality was 41% in patients with RV dilation compared to 11% in patients without RV dilation. On their analysis, RV enlargement was the only variable significantly associated with mortality.12
Pericardium
Case reports have described both pericardial effusion and cardiac tamponade as complications of myopericarditis in COVID-19.13,14
Point of care echocardiography has both high sensitivity and specificity for diagnosing pericardial effusion. The subxiphoid view is the easiest window for detecting pericardial effusion, as the most dependent portion of the pericardium is closest to the probe. In this view, pericardial fluid should be seen along the right heart border. In the parasternal long axis view, the most dependent portion of the heart is deep to the left ventricle, so pericardial fluid should be seen along the LV free wall. The pericardium is bound by the descending aorta, so pericardial fluid will track between the descending aorta and the LV, while pleural fluid will track posterior and lateral to the descending aorta.
In the setting of a large pericardial effusion and hypotension, assume the patient is in cardiac tamponade. If the patient is hemodynamically stable, it can be helpful to assess for echocardiographic signs of tamponade to anticipate the potential for decompensation.

Identifying a new pericardial effusion in the setting of COVID-19 suggests either pericarditis or myopericarditis. Use ultrasound guidance to treat cardiac tamponade with pericardiocentesis.
During this pandemic, both the ASE and the EACVI have empowered clinicians to use focused point of care echocardiography to improve the care of their patients with COVID-19.
Note: Images shown in this article are not from Clarius. Visit Clarius Cases to evaluate the image quality of our systems.
References
- Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Bondi-Zoccai G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol 2020; doi: 10.1016/j.jacc.2020.03.031.
- Johri AM, Galen B, Kirkpatrick JN, Lanspa M, Mulvagh S, Thamman R. ASE statement on point-of-care ultrasound (POCUS) during the 2019 novel coronavirus pandemic. American Society of Echocardiography 2020; available from: https://www.asecho.org/wp-content/uploads/2020/04/POCUS-COVID_FINAL2_web.pdf, accessed 28 Apr 2020.
- Skulstad H, Cosyns B, Popescu BA, Galderisi M, Salvo GD, Donal E, et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging 2020; doi: 10.1093/ehjci/jeaa072.
- Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020; doi: 10.1001/jamacardio.2020.1017.
- Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020; doi: 10.1001/jamacardio.2020.0950.
- Kim I-C, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J 2020; doi: 10.1093/eurheartj/ehaa288.
- Meyer P, Degrauwe S, Delden CV, Ghadri J-R, Templin C. Typical takotsubo syndrome triggered by SARS-CoV-2 infection. Eur Heart J 2020; doi: 10.1093/eurheartj/ehaa306.
- Bettari L, Pero G, Maiandi C, Messina A, Saccocci M, Cirillo M, et al. Exploring personal protection during high-risk PCI in a COVID-19 patient: impella CP mechanical support during ULMCA bifurcation stenting. JACC Case Rep 2020; doi: 10.1016/j.jaccas.2020.03.006.
- Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost 2020; doi: 10.1111/jth.14830.
- Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Research 2020; doi: 10.1016/j.thromres.2020.04.013.
- Li Y, Li H, Zhu S, Xie Y, Wang B, He L, et al. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. JACC Cardiovasc Imaging 2020; doi: 10.1016/j.jcmg.2020.04.014.
- Argulian E, Sud K, Vogel B, Bohra C, Garg VP, Talebi S, et al. Right ventricular dilation in hospitalized patients with COVID-19 infection. JACC Cardiovasc Imaging 2020; doi: 10.1016/j.jcmg.2020.05.010.
- Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020; doi: 10.1001/jamacardio.2020.1096.
- Hua A, O’Gallagher K, Sado D, Byrne J. Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J 2020; doi: 10.1093/eurheartj/ehaa253.