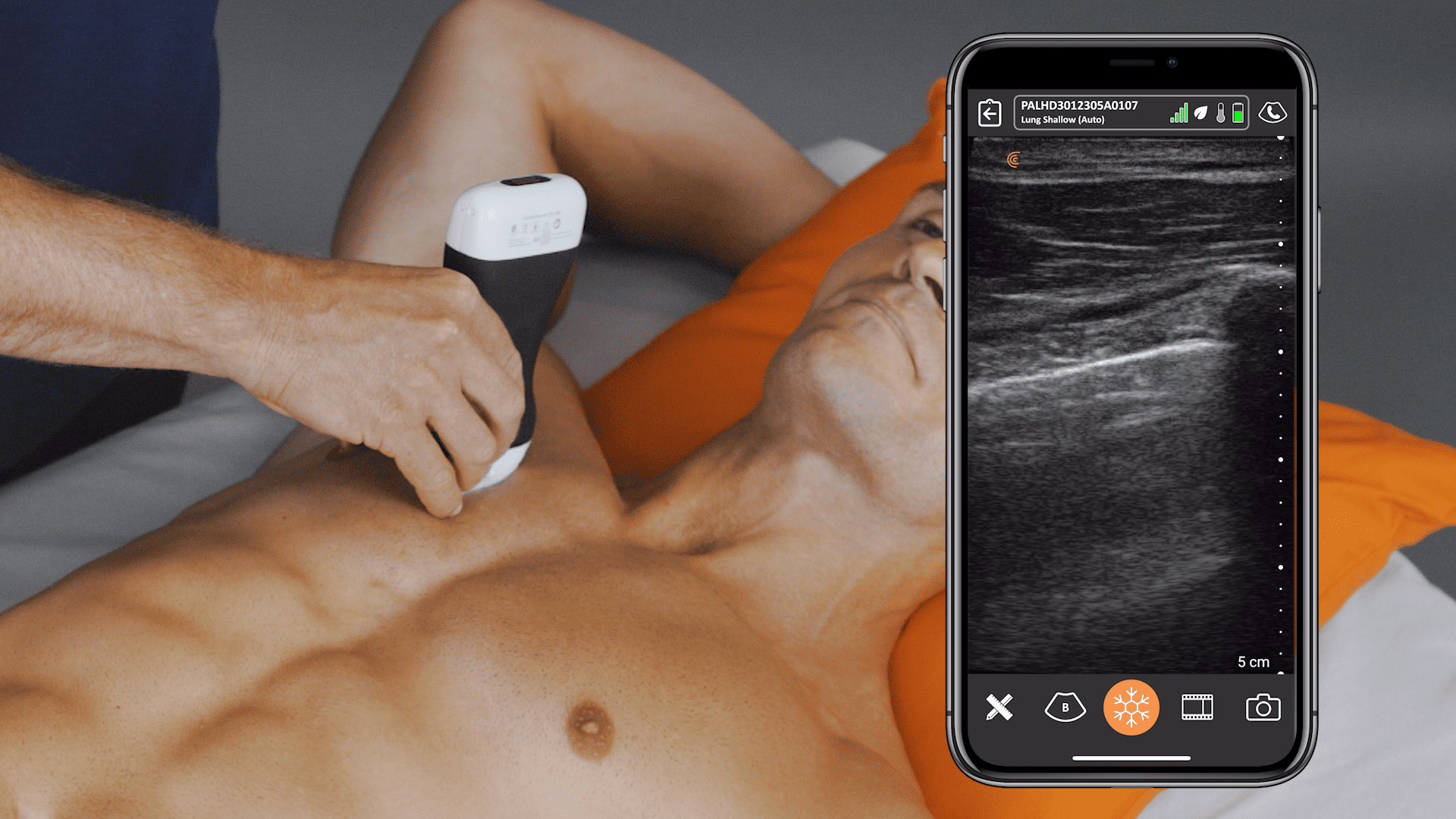
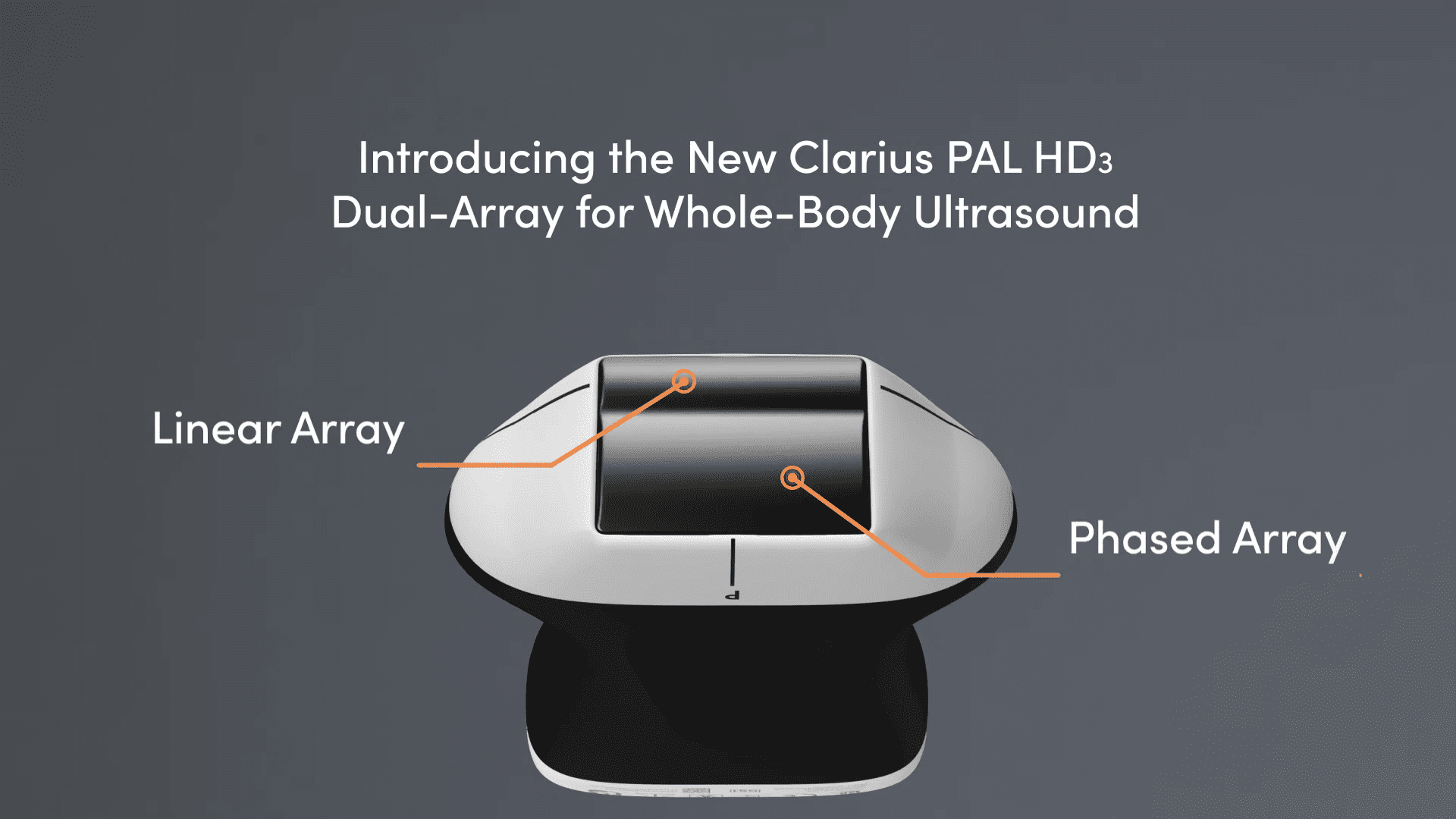
Point-of-care ultrasound (POCUS) is an essential tool for identifying the underlying cause of shock. Dr. Tom Cook, emergency physician, ultrasound educator and co-founder of 3rd Rock Ultrasound recently shared his knowledge and experience during the third webinar of a cardiac series: Cardiac POCUS Part 3: Resuscitation with Handheld Ultrasound. Watch the full webinar or read the blog for a quick review of Dr. Cook’s tips on using wireless ultrasound to perform the RUSH exam and improve patient management.
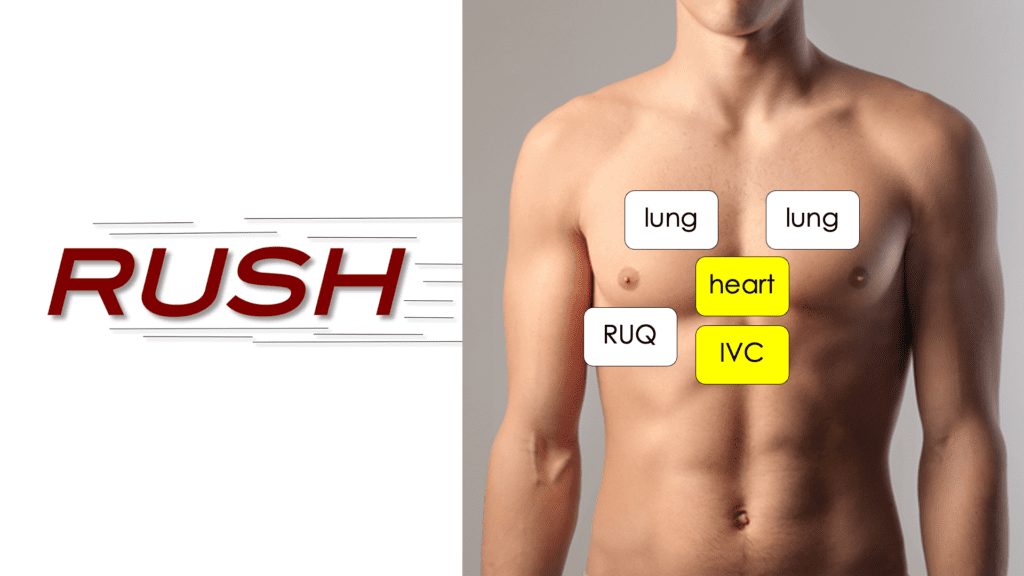
What Is the RUSH Exam?
RUSH stands for Rapid Ultrasound in Shock and Hypotension. The phrase was coined in this paper from 2010:
The exam has some similarities to the FAST and EFAST exams but focuses more on the heart and IVC. The components are the heart, inferior vena cava, the pulmonary system, and the peritoneum.
Shock Scenario in the ER
A patient arrives by EMS, breathing hard, sweaty, confused, tachycardic, hypotensive, and hypoxic. Is it the heart, the lungs, internal bleeding, or sepsis? The patient is in shock – how can ultrasound help?
What’s great about ultrasound is we can use this technology to, within a few minutes, help us with the diagnosis of what is could be, but more importantly, what it isn’t, to help us manage the patient effectively and go in the right direction, right from the get-go”.
Dr. Cook describes shock as a decrease in pressure in a closed vascular system, which is made of a pump and some pipes. There are four ways that can cause a decrease in the pressure within the vascular system.
- Pump (heart) failure – heart failure, valve disease, myocardial infarction
- Pipes leak – trauma, ruptured AAA, ectopic pregnancy
- Pipes expand – septic shock, neurogenic shock, anaphylactic shock
- Pipes blocked – pulmonary embolus, pericardial effusion, tension pneumothorax
The RUSH protocol will help quickly determine the type of shock and guide management.
How to Perform the RUSH Exam
Perform a rapid ultrasound to assess the following:
- Heart
- IVC
- Pulmonary
- RUQ
Watch this 4-minute video to see a demonstration of the RUSH exam
In as little as 2 or 3 minutes at the bedside with ultrasound we’ve
RULED OUT:
- Hypovolemia – dilated IVC
- Pneumothorax – pleural sliding present
- Massive pleural effusion – no fluid seen
- Large pulmonary embolism
- Intraperitoneal bleeding – no fluid seen
RULED IN:
- Heart failure – reduced LV function and dilated RV
- Hypervolemia – dilated IVC
- Pulmonary edema – B-lines
The cause of this patient’s shock, hypoxia, and respiratory failure is CARDIOGENIC SHOCK. Intravenous fluids will exacerbate the patient’s problem and cause harm, so the treatment choice is to manage with drugs.
Studies have shown that a POCUS ultrasound can improve diagnostic accuracy from just over 60 percent to 85 percent. To see additional shock scenarios and learn more about the RUSH exam, watch the free on-demand webinar, Cardiac POCUS Part 3: Resuscitation with Handheld Ultrasound.
About Dr. Tom Cook
Dr. Tom Cook is the founder of 3rd Rock Ultrasound, an education company designed to help all healthcare providers integrate ultrasound into their practices. 3rd Rock Ultrasound offers a variety of accredited ultrasound courses throughout the year to empower emergency and critical care physicians with the ability to utilize POCUS to improve patient care.