Amar Vira, MD, FACEP on Creating Value-Based Care Through Ultrasound
Amar Vira, MD, FACEP wears many hats: physician, educator, administrator. Being able to exercise many skill sets was one of the reasons why he chose emergency medicine — it has “a little bit of everything” and emergency physicians can apply their training to many different areas.
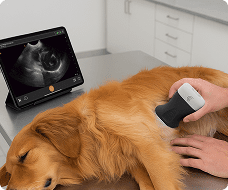
One of the tools he keeps by his side as an emergency physician is a portable ultrasound. “Point-of-care ultrasound, it’s a tool that we use in the ED that doesn’t take us away from our patient,” he explains in our newest podcast episode. “You learn something and bring it to the bedside. It really enhances the care that we provide every day.”
On a recent episode of our Healthcare Disruptors podcast, Amar talks about how clinicians should view point-of-care ultrasound as a helper and not a hindrance, and how ultrasound can contribute to more value-based healthcare.
Why POCUS shouldn’t be considered as « just another step »
As an emergency physician who uses ultrasound, Amar is convinced that clinicians shouldn’t see it as « just another step » to add to their already busy workday. Instead, « ultrasound, when used properly, enhances your throughput, enhances a patient’s experience, and then really enhances the patient’s quality and safety as they move through the ED into the hospital or home. »
As an example, he describes a patient who comes to the ED nervous about a pregnancy. Instead of getting immediate answers, they move about the hospital for testing and then wait — which can increase that anxiety.
However, Amar suggests we « flip that a little bit. You go see the patient, and while I’m talking to the patient, I’ve already pulled my ultrasound into the room. I’m ultrasounding the patient, I’m getting the history from the patient, examining the patient, and then doing my ultrasound right there at the bedside. They’re participating. I can show them what I’m looking at. I can, at the same time, do some education, show them some anatomy, and really let them be part of that process. And if the results of the ultrasound are positive, then I’ve relieved their stress and anxiety by the time I’ve left the room. »
Lowering barriers to ultrasound with earlier education
Amar is also dedicated to educating and mentoring others as well, and when it comes to lowering the barriers associated with learning ultrasound, Amar says it begins in one place: med school.
« At the med schools, they’re learning point of care ultrasound during their clinical years. So second year of med school, they’re putting their hands on the probes, they’re learning about cardiac anatomy. They’re learning it using a textbook. They’re listening to the heart sounds. They’re going to a cadaver lab and looking at the heart, but they’re also ultrasounding it,” Amar explains. “That is so key for learners is to learn it at that foundational stage. »
For today’s clinicians who received this training 10 or 20 years prior — or never did — it’s going to be hard to remember or learn. However, as med school introduces students to ultrasound and gives them practice on it, « you’ll see over the next 5, 10, 15 years, this is going to be ubiquitous. And I say this not just from an emergency medicine perspective. Cardiology, internal medicine, pediatrics, all specialties are really looking at point of care. »
A different approach to costs and value-based healthcare
Amar is also the medical director for Ascension, which has allowed him to get closer to hospital and healthcare administration and solve different problems in that capacity. One of the biggest challenges to healthcare systems today is costs, and reimbursements can be another hurdle to using point-of-care technologies. But, as Amar says, it all comes down to value.
« How do we add more value rather than just drive up those costs and try to maximize billing out of every little modality?” he asks. “Ultrasound is one of those things where … you have to look at the ROI, and not always in dollars, but the ROI, again, in these other ways. It’s the value, right? So how do we define the value? »
One way to provide value, he says, is by decreasing a patient’s length of stay in the hospital. If someone comes into the hospital for chest pain, they may need an ultrasound or echocardiogram as part of their work-up. It may be done that day or the next day, and once it’s read, 24 hours have passed. However, picking up an ultrasound probe and doing the scan in five minutes means getting immediate answers. « That would probably not reimburse as much as the comprehensive echocardiogram,” he says. “But if you were talking about value-based care, that patient’s length of stay just decreased by a day, and there’s a ton of value to that. Value to the hospital who are boarding patients and overcrowded, and value to the patient because they really want to go home. »
Conclusion
For Amar, it comes down to finding better ways to bring value to the patient — and one of those ways is through point-of-care technologies that allow for faster diagnosis, less time spent in the hospital, and less anxiety due to decreased wait times. Ultimately, it’s about educating and mentoring others, contributing to improving hospital systems, and giving back to the healthcare ecosystem.
Listen to the full interview with Amar Vira, MD, FACEP on the new season of our Healthcare Disruptors podcast.