We recently invited Dr. Marc Salzman, a double-board certified plastic surgeon, award-winning educator and Clarius user, to share his expertise. During a one-hour webinar, he took us through three cases, including one where he shared how handheld ultrasound is quick and safe for the surveillance of silent breast implant ruptures. He next discussed how handheld ultrasound helps him diagnose and treat common post-surgery complications, in particular, abdominal seromas.
We invite you to watch a recording of the full webinar to explore all three cases. Or, read on to learn what Dr. Salzman says about how to use handheld ultrasound to help diagnose and treat abdominoplasty seromas.
With handheld ultrasound, I can quickly diagnose the reason for post-op contour irregularities.
I see a lot of contour irregularities, both in my patients and other people’s patients, early post-op. This is a very common problem, experienced by 77% of the plastic surgeons who participated in the live webinar poll:

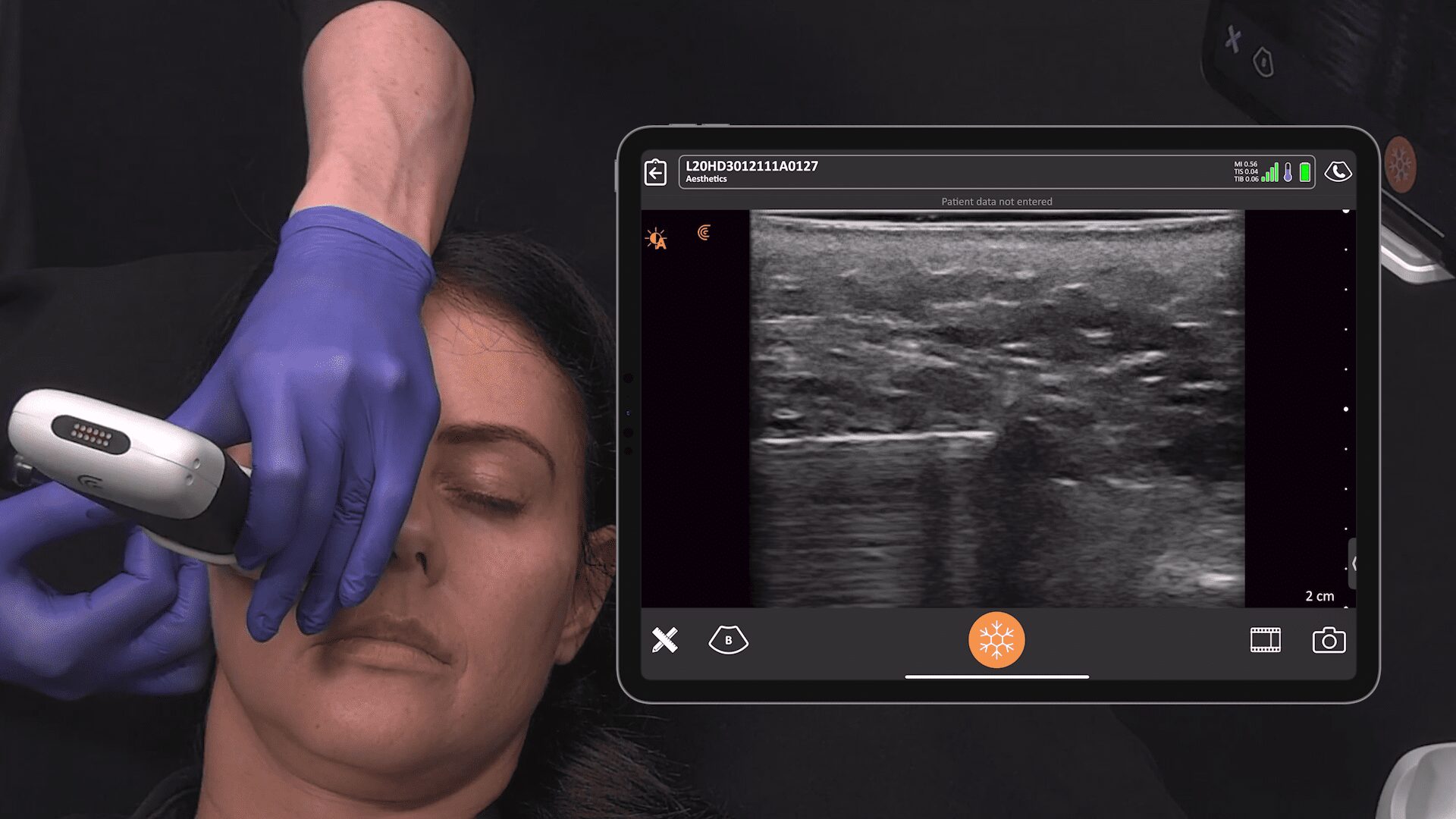
On the surface, contour irregularities could be caused by a seroma or hematoma. To see the what’s going on, I use a little Clarius handheld ultrasound device that’s readily available – either in my pocket or in the room where I’m seeing the patient.

In this case, my patient is a woman who was operated on by another surgeon. She had a persistent contour irregularity after an abdominoplasty and mastopexy with implants. I saw her several months after surgery. A radiologist had aspirated 280 cc. And then aspirated 40 more a few months later. By the time I saw her, she had this seroma.

As you can see in the video shown above, I aspirated the seroma. The red dots are along the needle. You see the needle come into the cavity. What’s really cool is you can watch the black, or the hypoechogenic fluid, slowly get closer and closer so that the black is gone, and the regular, lighter-colored soft tissues are coalescing. It’s quite satisfying to see that.
The seroma was stubborn and came back, such that she ended up with the lump pictured below, which was located just above her belly button.

On the day of surgery, I didn’t want to go through the tummy tuck incision and go all the way up to cut it out. It had been there for almost a year by now and aspiration wasn’t working. So, I scanned with ultrasound and saw that I was actually dealing with a pseudo-bursa, as shown below:

On the ultrasound, you see the hypoechogenic center. If you look just beyond where the black is, it looks a little fuzzy. Then, there’s this dense, fibrous tissue that doesn’t have the normal architecture of fat. When you see this white matter, it is scar tissue that’s mixed in with the fat. A pseudo-bursa is when scar tissue forms around a water-filled sac.

Above is what the pseudo-bursae looked like on ultrasound. You can see the capsule – it’s a dense, echogenic signal. And then you have a hypo echogenicity, or almost no echo at all, because it is fluid filled. This is actually basic, first level ultrasound image interpretation. Black is fluid wherever you see it and the white is dense, fibrous tissue.
Comparing excised pathology to the pre-surgery ultrasound helps build diagnosis confidence.


With a side-by-side comparison, you can see how ultrasound clearly shows exactly what will be found after opening up the patient.
The clinical course was to excise the pseudo-bursa and close it over a small drain. On the right, this is what the pathology looked like. And on the left, we can compare what it looks like on ultrasound. The thick white matter is this sclerotic looking fat. The pseudo-bursa is the anechoic center representing fluid, which is the black. Occasionally we see a light echogenic lining representing the hyalinized mucosa.
Monitoring with ultrasound post-surgery helps avoid complications.
In summary, high-resolution ultrasound imaging is useful to evaluate and treat post-abdominoplasty contour irregularities. Persistent seromas may become pseudo-bursae that necessitate excision. And you’ll know that by monitoring them over time.
If they have an early contour irregularity, you can differentiate hematoma from seroma. You can aspirate seromas. You can wait for your hematomas to be totally black in the middle. If you start seeing some more echogenicity in the center of your hematoma and it’s organized, it’s a clot. It’s not going to come through a canula. So, you’ve got to wait 10 to 14 days, put warm soaks on the area. Then, you can drain it out and you won’t get a pseudo-bursa. If you leave them for too long, you’ll end up with issues like we’ve just explored. Using an ultrasound scanner to monitor post surgical developments really helps to prevent late complications.
Scanning every patient with ultrasound is the best way to learn.
When I first started using ultrasound, I looked at every single tummy tuck right after we finished to see what it looked like. And when patients came back on day seven. Can you guess how many had seromas? 100%! Every patient had a seroma, but they were not clinically relevant. If you follow your patient’s recovery with ultrasound, you’ll be so surprised at what you see. You’ll see little 3 x 1 cm collections. But they are very small and inconsequential. These will reabsorb on its own, and don’t require us addressing it.
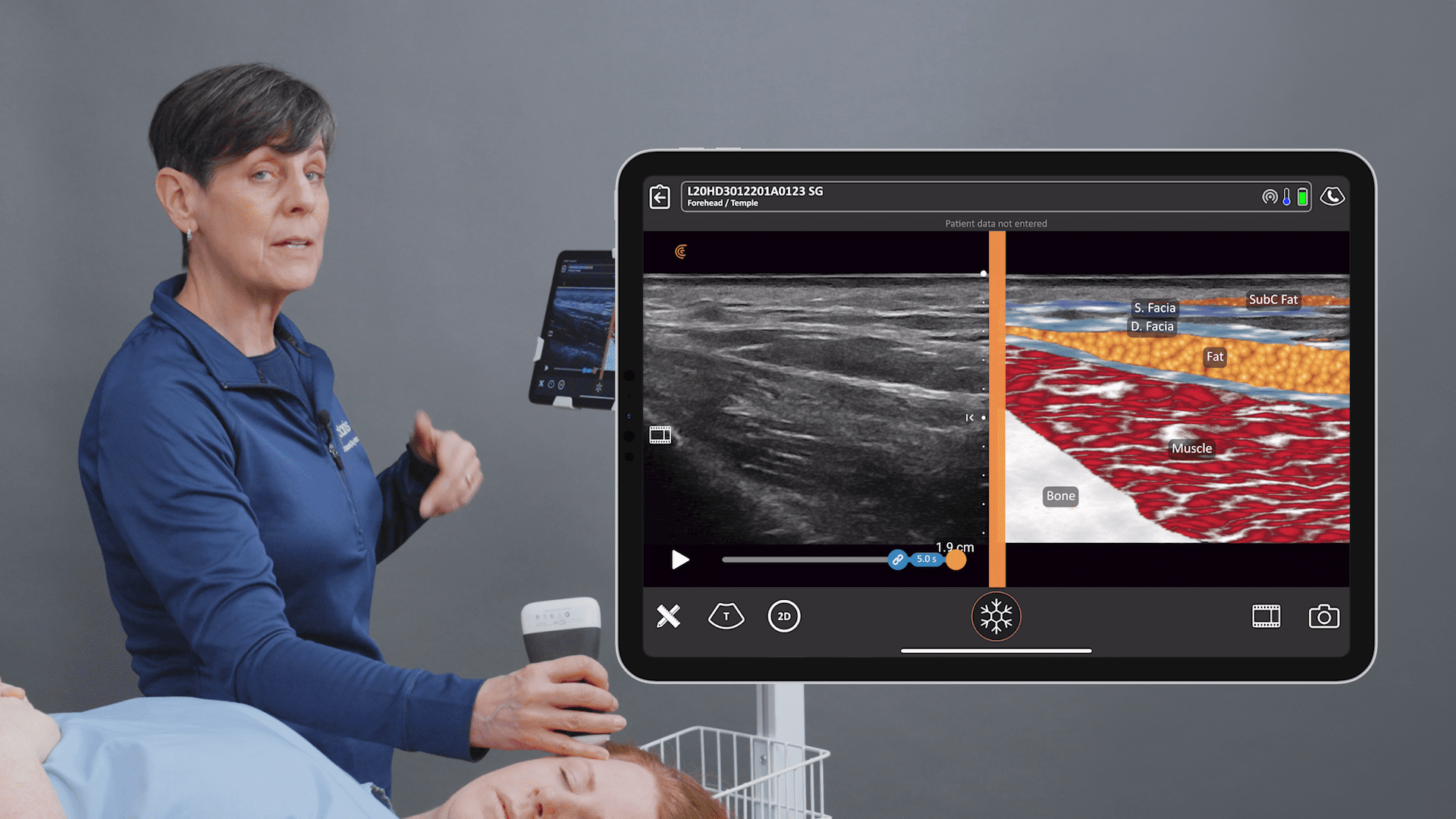
It’s important to scan everything when you first start so you learn what you’re seeing by correlating real anatomy with the ultrasound image. That’s what I did – it was fun and novel! I scanned everything because I didn’t know what it looked like, nor what it was supposed to look like. Lots of scanning with my handheld ultrasound helped me learn very quickly.
______________
Based in Louisville, Kentucky, Dr. Salzman has been practicing since 1992. He lectures online and around the United States on his innovative techniques, including lecturing for plastic surgery residents at the University of Louisville.
Dr. Salzman has been using ultrasound since 2012. He switched from a laptop ultrasound to the Clarius L7 HD in 2019. Read his article here about why ultrasound is essential for every plastic surgeon.
To learn more about how easy and affordable it is to add Clarius HD to your plastic or cosmetic surgery practice, contact us today or request an ultrasound demo to see the difference high quality imaging makes.