Dr. David Rosenblum, Director of Pain Management at Maimonides Medical Center in New York, recently demonstrated three pain management procedures in a webinar hosted by Clarius. In this post, Dr. Rosenblum shares how he treats patients for chronic knee pain using nerve blocks. To learn more, watch a recording of the full webinar including guidance on which CPT codes to use for reimbursement in the United States.
Case 3: Ultrasound-guided Injections for Chronic Knee Pain
When I started my pain practice, I met some resistance from other pain doctors on using ultrasound in the office. They wondered what I was going to do with it. My response was that I treat almost anything and everything with ultrasound.
I get better results for my patients and in many cases I can bill for ultrasound. It has added a dimension to my practice – a competitive edge.
A knee injection is one that a lot of physicians are taught to do blind. It’s an easy procedure for physicians who are starting to use ultrasound. You see a dramatic leap in the quality of your results.
Patient Background
A 73-year-old patient presents with bilateral chronic knee pain. He asks about injections of the knee, having already tried steroids and a visco supplement. He suffers from coronary artery disease as well as COPD.
He has significant past surgical history of right arthroscopic meniscectomy. It’s very common for patients to still have arthritis after the procedure. He has knee pain and crepitus is present on the knee exam with flexion bilaterally. There’s also tenderness on the medial aspect of the joint, and it’s negative for drawer’s sign. His orthopedic has advised replacement, but the patient wants alternatives.
In my pain practice, typical alternatives to steroid or visco supplements include a genicular nerve block. I’ve done countless saphenous nerve blocks. I’ve done PRP, I’ve done mesenchymal stromal cells and bone marrow aspirate, and I’ve also done neuromodulation placing wires on the saphenous or genicular nerves. These can be implanted either temporarily or permanently.
First, a Review of Knee Anatomy
Of note on the diagram below are the sciatic nerve, the tibial nerve and the common peroneal nerve. Perhaps more relevant for the knee, you also have a saphenous nerve, the infrapatellar branch, which is amenable to nerve blocks, cryotherapy, lesioning or neuromodulation to treat nerve pain.
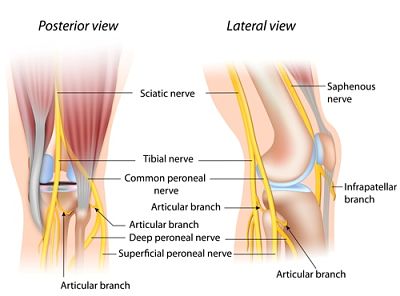
There is also something called the iPACK block, which is a nerve block that I do under ultrasound where I place a needle between the tibial nerve and artery and the actual posterior capsule of the knee joint. This is a highly effective way to treat for posterior capsule pain of the knee.
Taking Off the Blindfold to Simplify Procedures
On the image below, we clearly see the patella tendon and the tibia. The femur is up north. If you look at the slanty line, it points to the ACL. This is the ultrasound on the anterior aspect of the knee or the right sagittal view of the anterior aspect of the knee, which is why you can see the ACL.
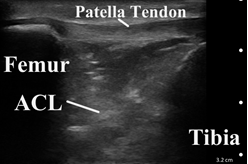
Under ultrasound guidance, an injection can be done easily in a multitude of ways. You can come in plain transverse, with the knee bent and the patient sitting. Or you can have a nice straight leg and come from above.
In the video below, I come in out of plane. I use the ultrasound to avert contacting the bone, avoiding unnecessary pain for the patient. I insert the needle after I find my anatomy. As you can see in this older video, I can see my whole needle trajectory.
Genicular Nerve Block – A Black Belt Procedure
The genicular nerve block and the suprascapular nerve block are two blocks that really changed my practice about five or six years ago. It takes experience with ultrasound to perform these blocks, but the results are undeniable.
I’ve seen patients get amazing relief from the genicular block, after years of suffering because nothing else worked. For some patients, I terminated their seven-year pain problem, permanently, with just one shot.
There was a time when there was nothing I could offer patients who had pain after a knee replacement, except the saphenous nerve block. Then I experimented with the genicular nerve block – though it wasn’t standard, the results were night and day. When patients came back to me, they came for other problems; they no longer complain about their knee.
There’s a lot of disagreement in the literature as to the origin of the genicular nerves. They are a group of nerves that innervate the knee. If you know where to do the nerve block and the proper ways to do it, you can deliver significant paint relief. A word of warning: don’t target the inferior lateral genicular nerve because you’ll cause « foot drop. » You can do this block effectively under x-ray or ultrasound, though I’ve found it’s easier with ultrasound. Let’s review the anatomy.
An X-Ray of AP Genicular Anatomy
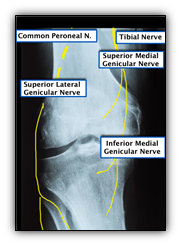
This X-Ray image shows the superior medial genicular nerve, coming from the tibial nerve. It passes over the medial epicondyle of the distal femur. You also have the inferior medial genicular nerve branch and the superior loud iniquity nerve branch coming from the common peroneal nerve.
Lateral Genicular Anatomy
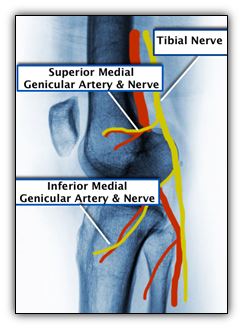
In the lateral view above, you see the nerves running with the blood vessels towards the joints. You have the superior medial and the inferior medial.
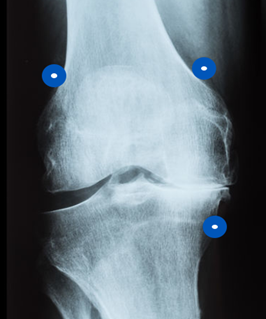
Traditionally, your targets were the blue points in the x-ray above. You came in from an AP View and then checked your lateral view. The vastus intermedius branches of fourth potential target above the patella. Most people no longer use it, but it’s good for sub patellar pain.
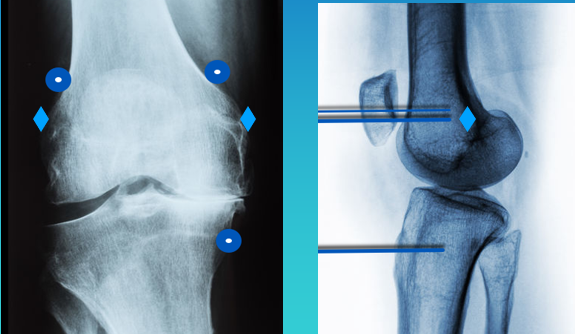
Above, I’ve marked diamonds for the revised recommendations. A lot of physicians are now recommending we do the blocks there. On ultrasound, I have been able to trace the nerve to confirm the new recommendations. The nerve is more superficial and there’s less soft tissue between your probe and the target, so it’s easier to do the block.
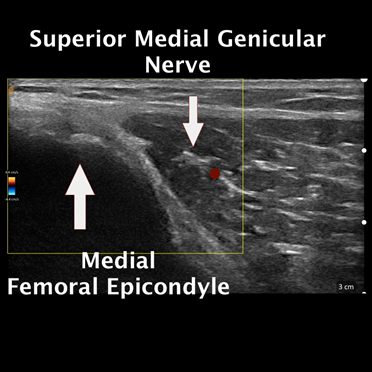

In the ultrasound image above, with the probe oriented longitudinally and coming from the inside, we visualize the shaft of the femur and the epicondyle. You can see the right dot, showing the artery next to the nerve. This is a very clear image. The nerve is not always as circular, it can be oval or even long. It’s takes a different course and it changes direction. It may appear larger, smaller or longer. The look of the artery also varies.
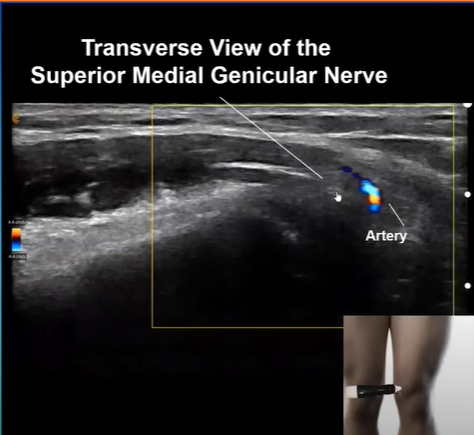
This ultrasound image showcases the Aryan seat. The artery looks a little different, as I turned the probe horizontally. The nerve is the adjacent structure, where I positioned the pointer at the end of the white line. It’s really very tiny. The general rule is these nerves run along the blood vessels, so if you inject within one or two millimeters, the pain medication will spread in this vicinity to bring your patient relief.
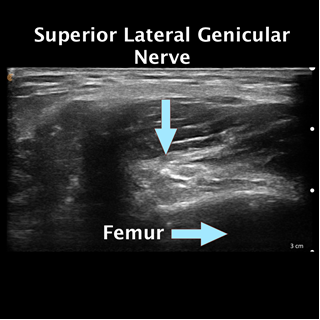
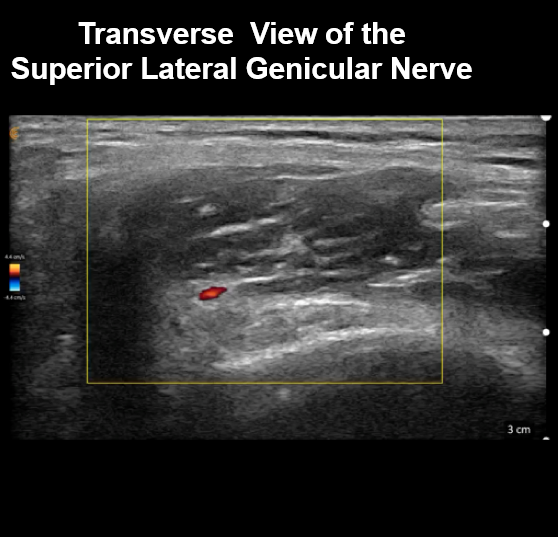
You don’t need a lot of volume as your injections become more precise with ultrasound guidance. You also make the procedure less painful for patients. Historically these procedures were just done with C-Arm or fluoroscopy. Sometimes we would even sedate patients to avoid procedural pain. Today, we have ultrasound. Below we see the transverse view of the superior lateral genicular nerve. Such clear imaging helps us perform more accurate injections, reducing both risk and discomfort.

Using Handheld Ultrasound to Facilitate Genicular Nerve Block Procedures
I use the Clarius L7 HD high frequency handheld ultrasound for my practice, which works well for all of ultrasound-guided pain management procedures, both shallow and deep.
Watch the following video to see Dr. Rosenblum in action performing a genicular nerve block.
A prolific educator, Dr. Rosenblum hosts the Pain Exam Podcast and created a Pain Exam Board Review, which has helped over 3,000 pain management physicians become board certified. Visit the Pain Exam website to learn about upcoming CME-certified pain management courses.
Interested in learning more from Dr. Rosenblum? You can review his case about plantar fasciitis and hip pain here.
To learn more about the advantages of Clarius HD, visit our wireless ultrasound for pain management page or watch a full recording of the Dr. Rosenblum webinar to explore best practices for guided injections.