Dr. David Rosenblum, Director of Pain Management at the Maimonides Medical Center in New York, recently demonstrated three pain management procedures during a live webinar hosted by Clarius. Read on and watch a video to learn how Dr. Rosenblum treated a patient for hip pain. Or watch a recording of the full webinar, including guidance on which CPT codes to use for reimbursement in the United States.
Case 2: Hip Pain Overlying the Greater Trochanteric Bursa
Patient Background
A 67-year-old female presented with right hip pain. She has a history of diabetes and hypertension and has had an appendectomy in the past. During the exam, the patient had slight pain on internal and external hip rotation with the joint flex. She had marked tenderness overlying the Greater Trochanteric Bursa. The bursa injection can feel like a maze.
A Review of Hip Anatomy
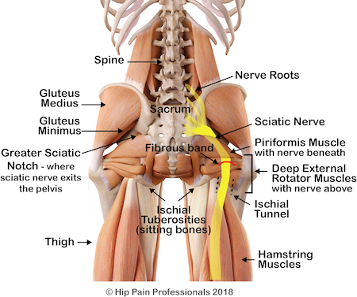
Let’s start with a quick review of some anatomy. You have the Bursa to the side of the greater trochanter. First, where you have the insertion points of the gluteus medius tendon, you have the hip external rotators. You have the sciatic nerve, the L4/L5 nerve roots and anterior to the posterior sacrum. You have the sacral roots all forming the sciatic nerve. You can see the piriformis and its relation to the sciatic nerve, which is very important for piriformis syndrome and even the hamstrings. Every now and then, I’ve even been fooled when I see a patient with hamstring tendonitis and they present like a sciatica patient. In these cases, the ultrasound can help identify pathology as well as guide the needle.
The Anterior Approach for Hip Injections
In general, when we talk about hip injections with the ultrasound, I prefer the anterior approach. It’s more superficial and I can see the femoral artery nerve and vein so I can avoid them. I think it’s less painful as well. The posterior approach is typically what I would use with a CRM or an x-ray and with a very obese patient when I don’t feel comfortable using an ultrasound.

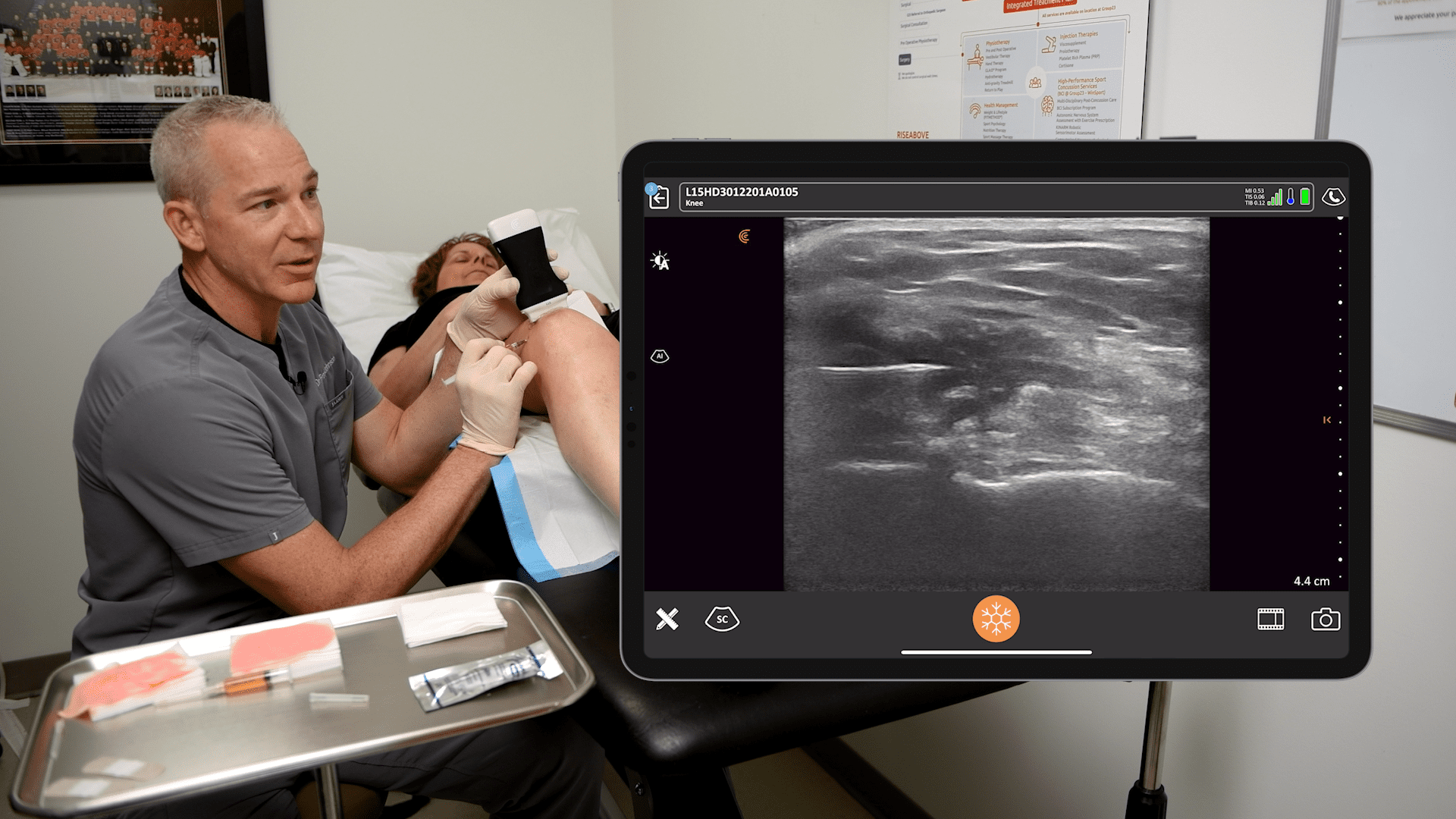
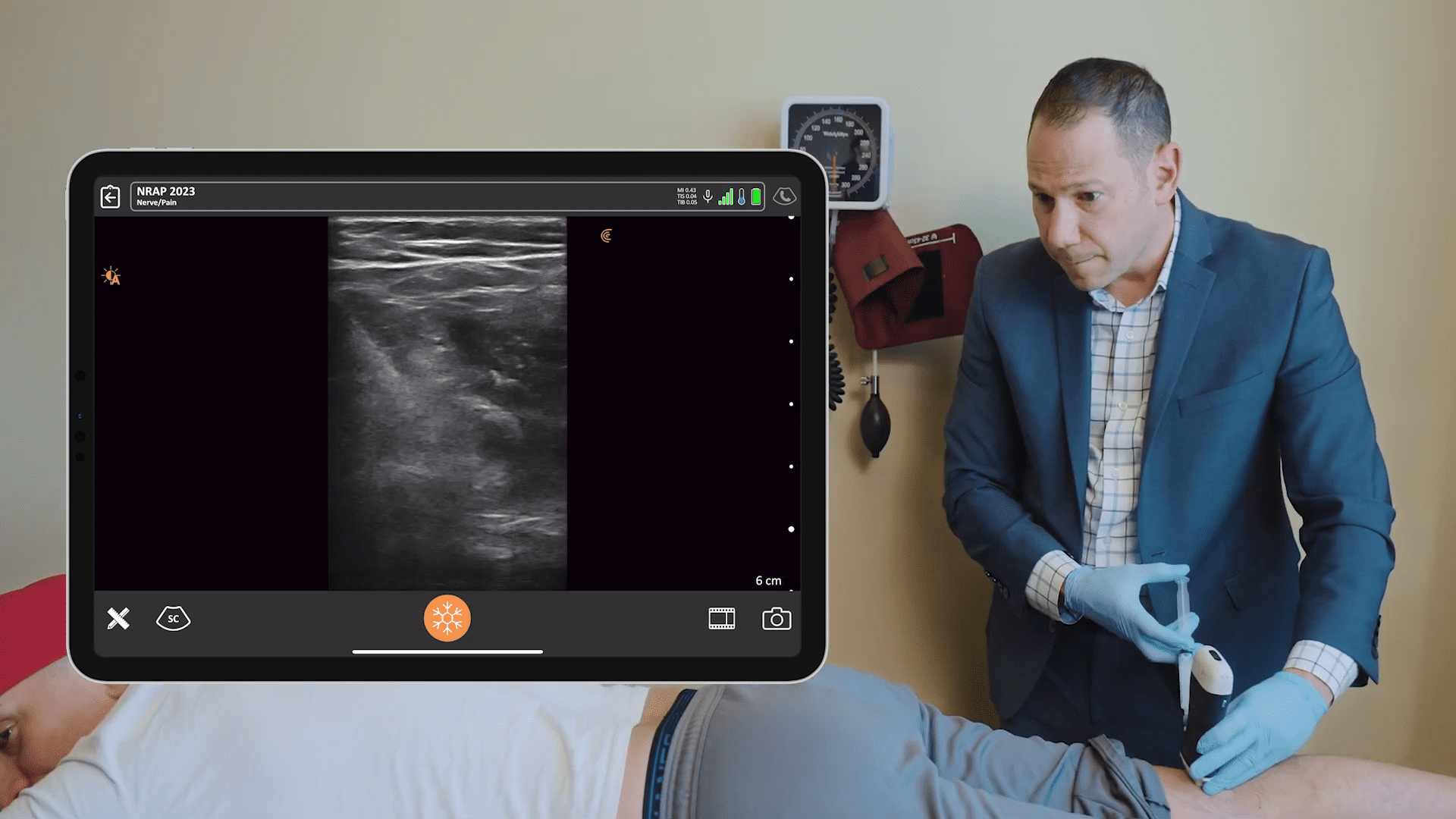
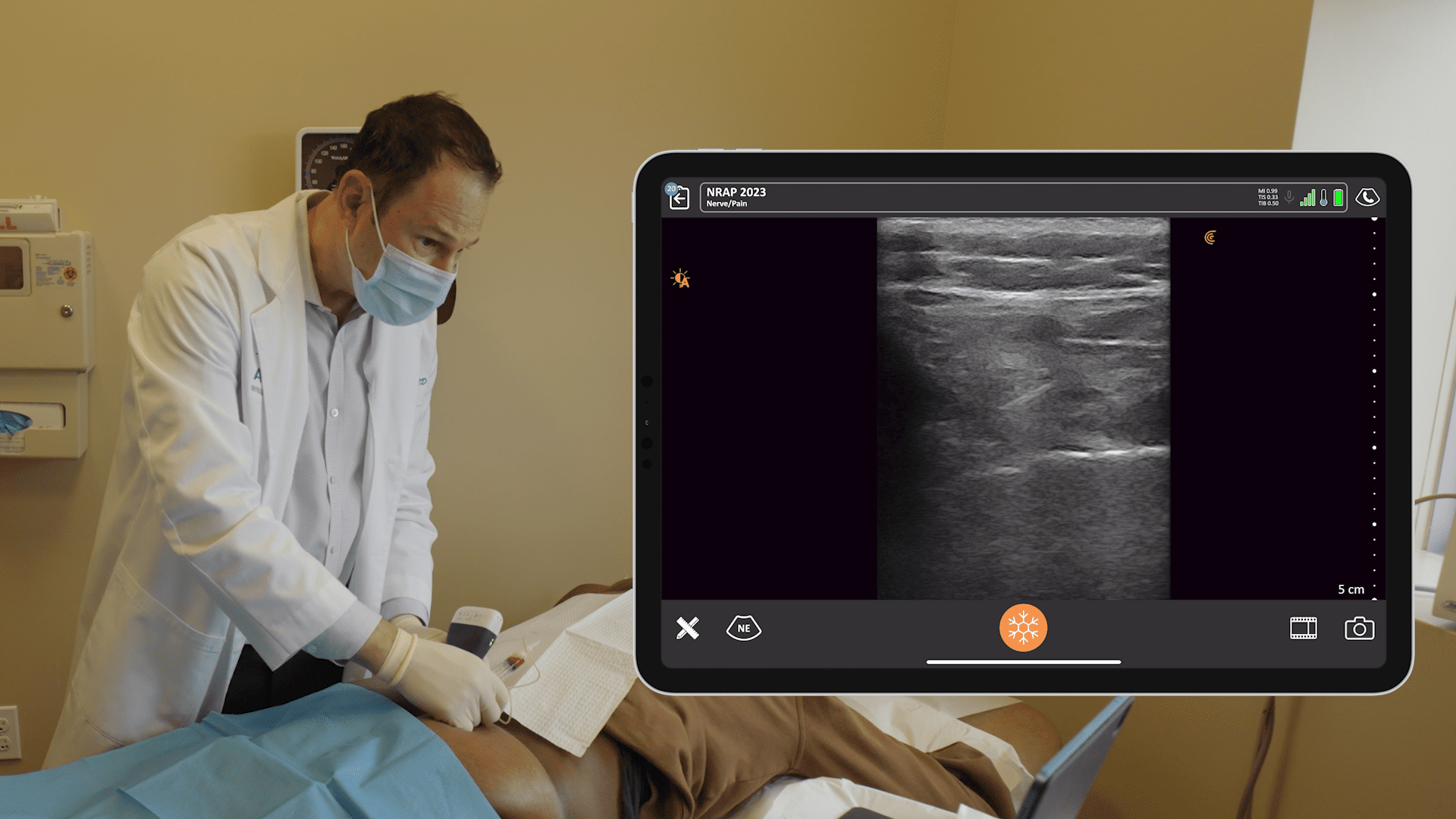
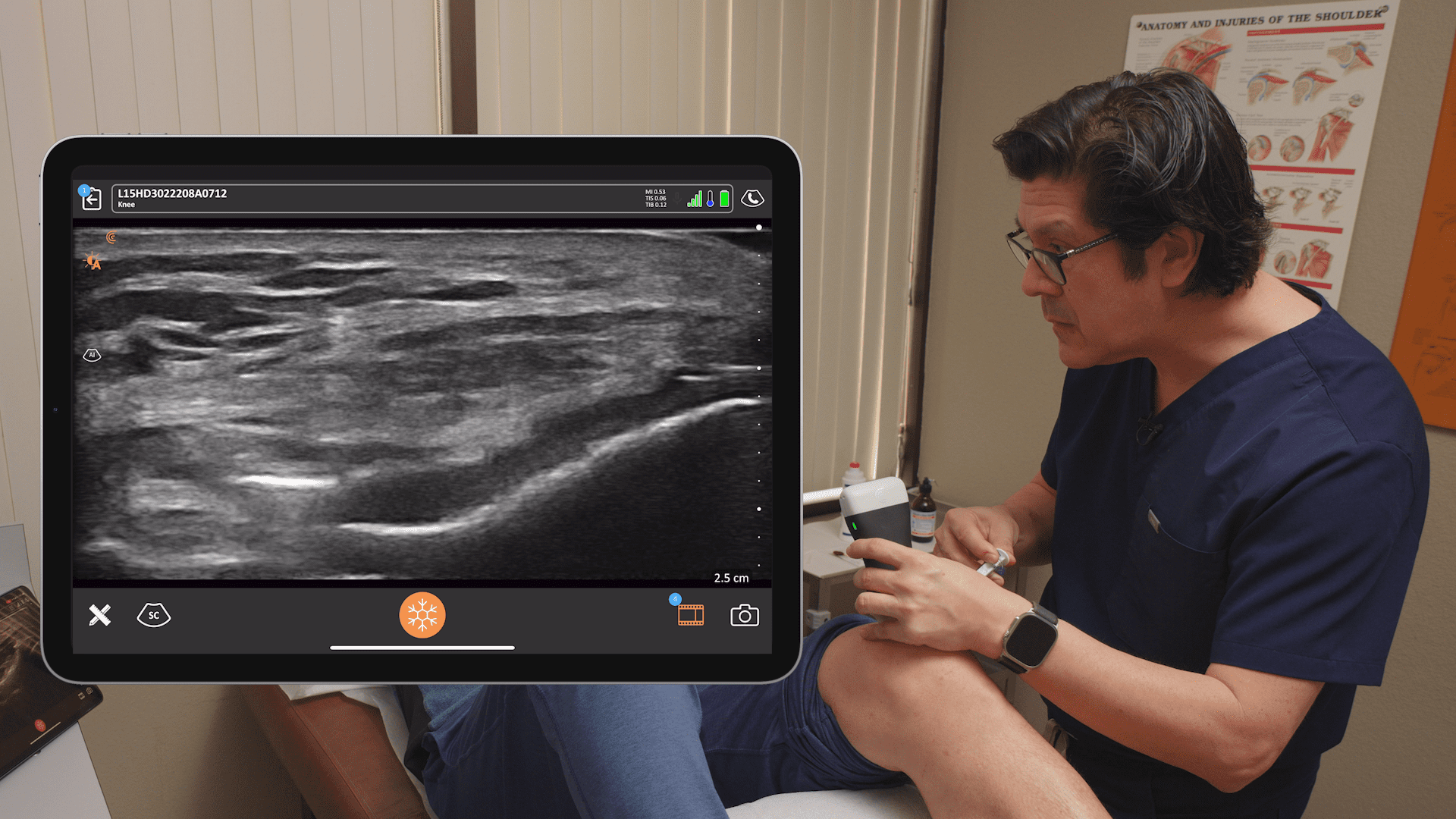
These days, I use the Clarius ultrasound, because the resolution is so good with the L7 high frequency scanner, which lets me see down to 11 cm. It’s usually no more than 6 cm deep, maybe 7 cm on larger patients.
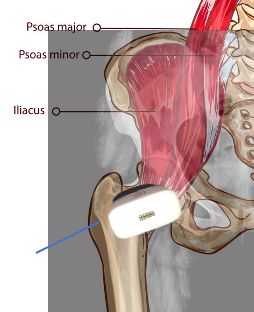
How do I typically position the ultrasound? I’m trying to go, not necessarily lateral, but more like an oblique to get into the line of the neck of the femur to visualize the head. The key is to see the neck and the head, with the iliopsoas muscles and tendons overlying the hip joint.
Unlike a lot of other joints, with the hip joint you’re not aiming at that hyper loose space. You’re actually aiming at the head, which I show you in the video because there’s bone there and it interferes with your access to the joint.
Watch the video to see Dr. Rosenblum guiding a hip injection under ultrasound guidance. Dr. Rosenblum uses a vapor coolant spray to anesthetize the skin and a 25 gauge three and a half inch final needle, which is less painful.
On Deciding Where to Treat Hip Pain
Often a patient will present with symptoms related to sacroiliac joint pathology along with the Bursar or hip joint pathologies. Deciding between a greater trochanter injection versus the hip joint depends on what the patient describes as more tender at the time of presentation. Sometimes hip pain in patients will radiate to the groin. Or pain will radiate down the leg towards the knee. Sciatica is common with hip pain. There’s a lot of overlap of these syndromes.
Sometimes the only way to make a diagnosis is to do a diagnostic injection, possibly into the SI joint or the hip joint and see if they feel better. In this case, intervention is actually diagnostic. There are times when I just give lidocaine into the hip and the patient feels amazing, which is great confirmation, because I don’t want to use steroid unless I’m 100% sure what the pathology is.
Dr. Rosenblum uses the Clarius L7 high frequency handheld ultrasound scanner for his practice, which he says works well for all of his ultrasound-guided pain management procedures, shallow and deep. He has been a Clarius user since 2017.
A prolific educator, Dr. Rosenblum hosts the Pain Exam Podcast and created a Pain Exam Board Review, which has helped over 3,000 pain management physicians become board certified. Visit the Pain Exam website to learn about upcoming CME-certified pain management courses.
Interested in learning more from Dr. Rosenblum? You can review his case about plantar fasciitis here.
To learn more about the advantages of Clarius HD, visit our wireless ultrasound for pain management page or watch a full recording of the Dr. Rosenblum webinar to explore best practices of guided injections.