You need quick answers about cardiac function in your patient presenting with chest pain, dyspnea, or unstable vitals. How can cardiac POCUS help? Dr. Tom Cook, emergency physician ultrasound educator and co-founder of the 3rd Rock Ultrasound, shared his insights in a recent webinar: Cardiac POCUS Part 1: Techniques for Assessing Left Ventricular Function. Watch the full webinar or read on to learn four very simple ultrasound techniques to quickly evaluate the left ventricle and determine the next steps in the management of your patient.
Common Scenario in an ER
An older patient presents to the ER with abdominal pain and a history of rectal bleeding. And by the way, his doctor mentioned that he has heart failure. Vitals indicate he’s in shock – tachycardic and hypotensive, and he has low hemoglobin. He needs volume resuscitation with blood, but with his lingering story of heart failure, the big question is “can this guy’s heart take it?”
A quick focused echo only takes a few minutes, and Dr. Cook demonstrates four techniques to both qualitatively and quantitatively assess this patient’s left ventricular function and determine the next best steps.
- Myocardial Thickening
- E-Point Septal Separation
- Fractional Shortening
- MAPSE
Myocardial Thickening
The heart muscle is like other muscles in the body. Normal muscle does two things – it gets shorter and thicker with each contraction. This can be easily assessed from the parasternal and apical windows, and there are no measurements needed.
This video shows a nice comparison of normal and abnormal myocardial thickening.
E Point Septal Separation
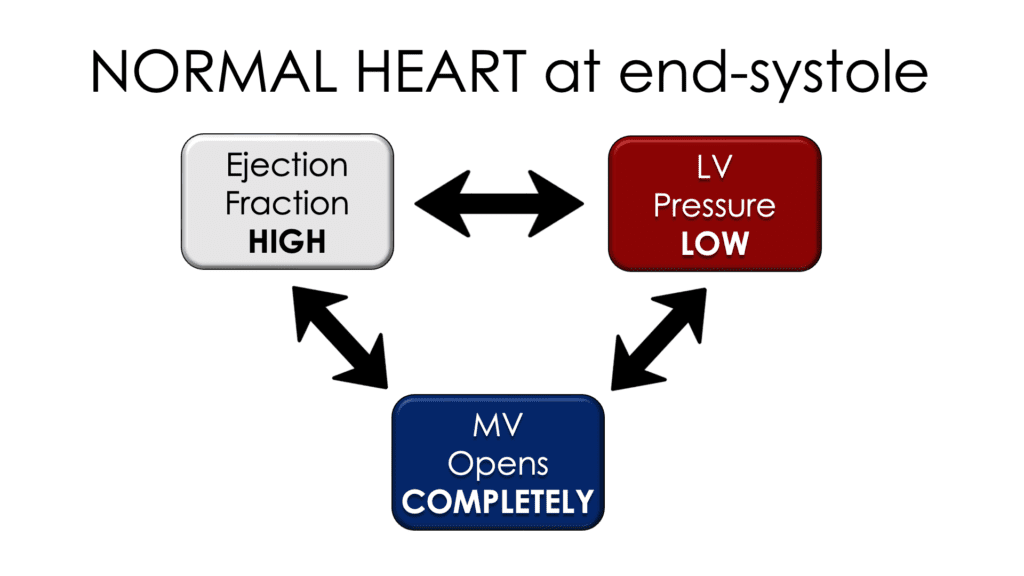
The anterior mitral valve leaflet is large and anterior, making it easy to see with ultrasound. The excursion of the leaflet can be a very useful tool in evaluating LV function. In a heart with normal LV function, when the valve opens in diastole, the anterior leaflet comes near to or even touches the interventricular septum.
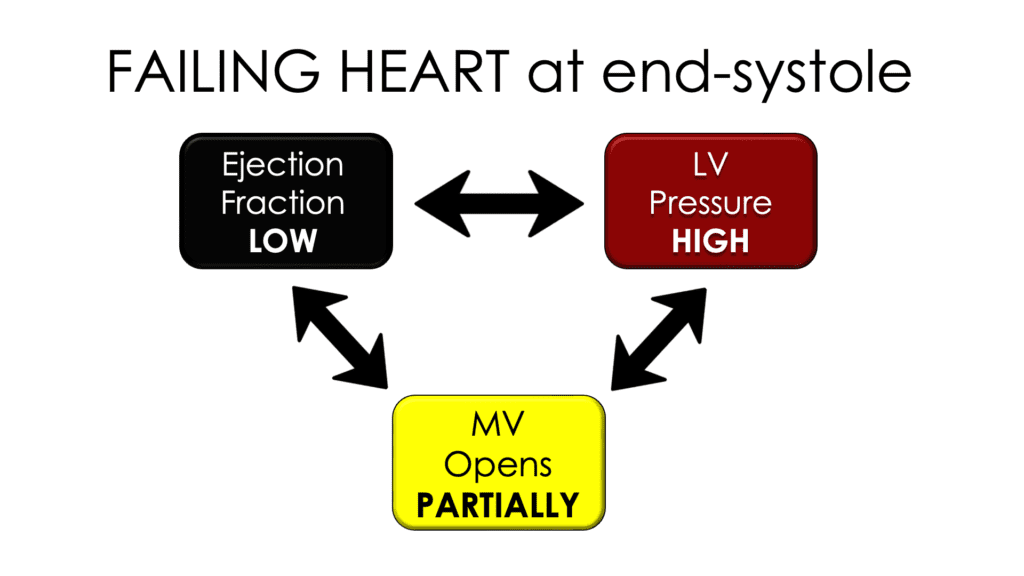
How can this be used to assess function? In a normal heart, the pressure in the left ventricle is very high at the end of diastole because it’s filled with blood. After systolic contraction, when most of the blood has been pumped out through the aortic valve (normal ejection fraction of 60%), the relative pressure in the left ventricle is low. In a normal heart at the end of systole, we know the left ventricular pressure is relatively low. That sets up a big pressure gradient between the atrium and the ventricle, and that allows a large quantity of blood to move from the left atrium into the left ventricle. In early diastole, the mitral valve opens all the way for this to happen. Therefore, if the mitral valve opens completely, the ejection fraction will be high.
In the failing heart, pressure gradient between the left ventricle and atrium, which means there’s a smaller amount of blood moving across the mitral valve, and the valve will not open fully. This indicates a low ejection fraction.
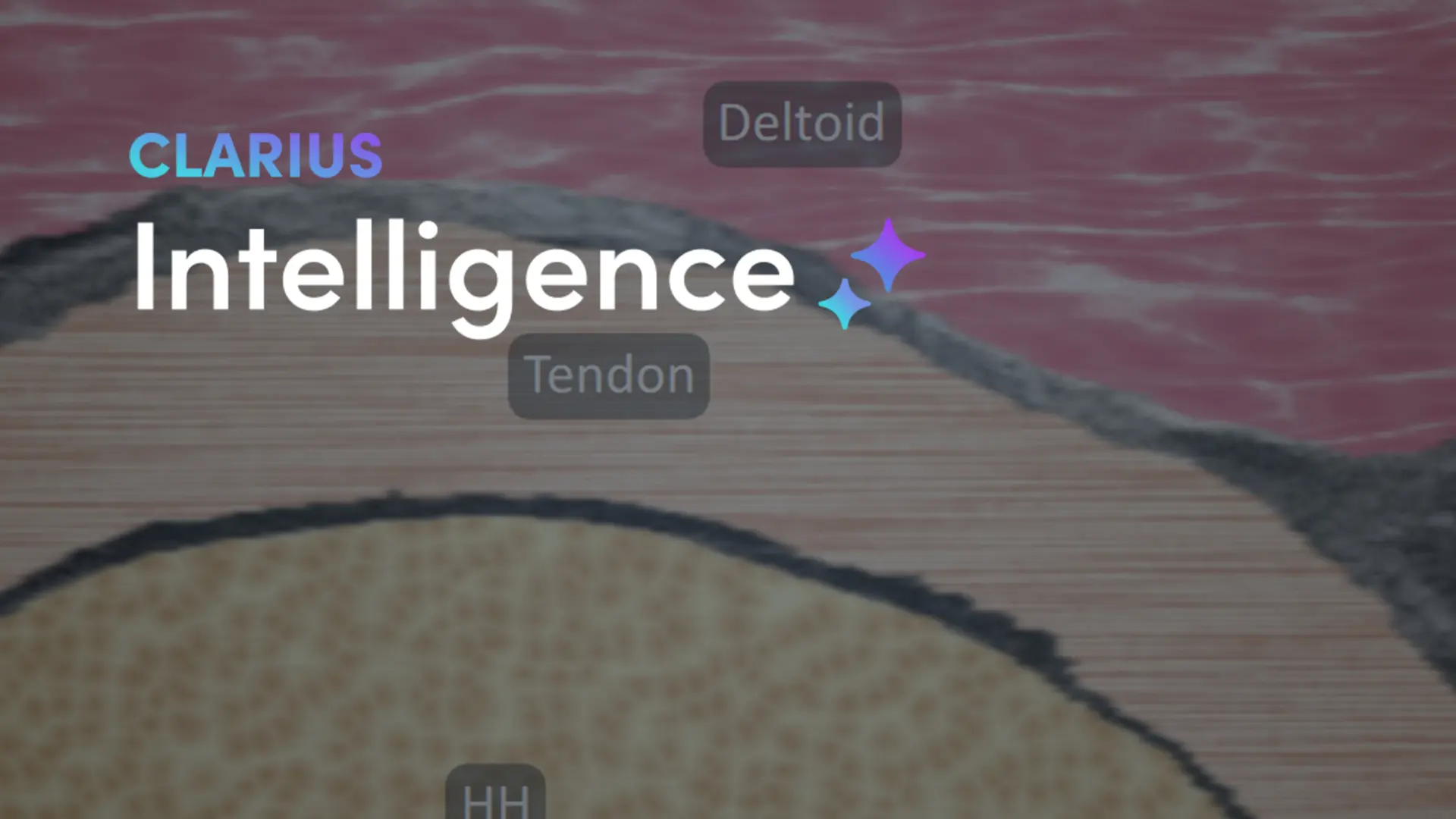
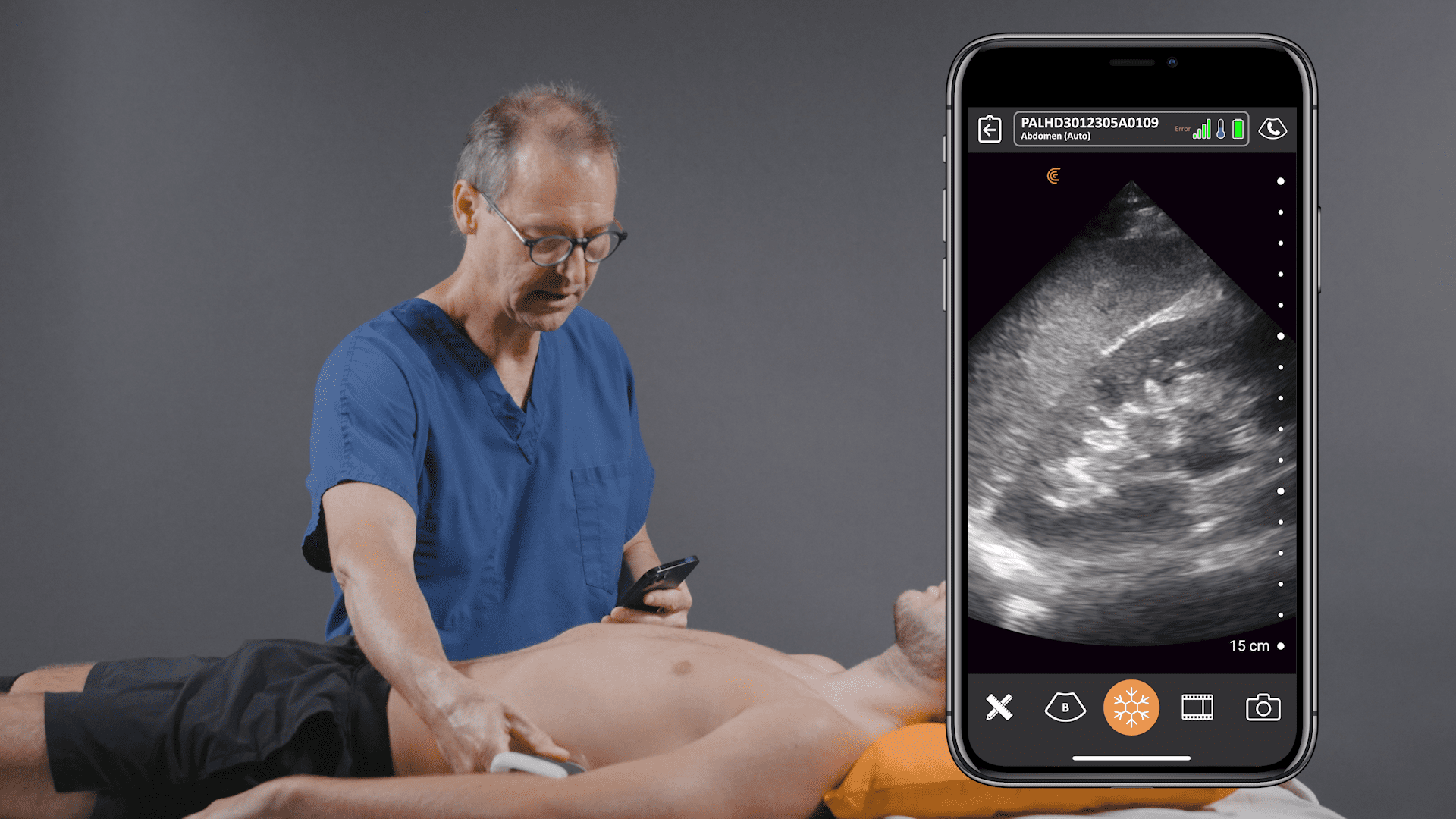
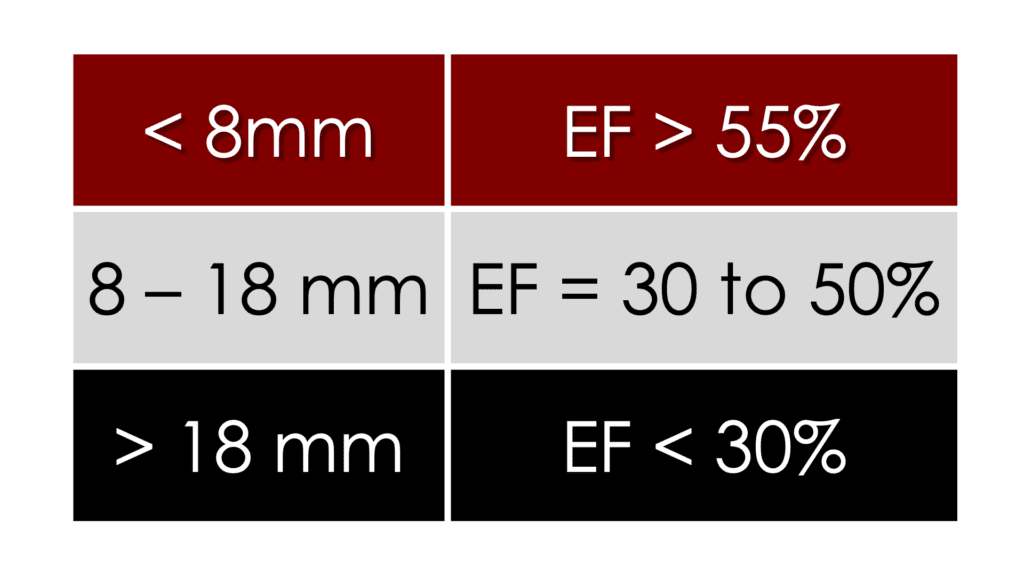
This can be quantified in a measurement called E-point septal separation, or EPSS. Dr. Cook describes the measurement and how it’s done using an m-mode with the m-line placed across the tips of the mitral leaflets. Watch this video to see Dr. Cook’s demonstration on an EPSS measurement using the Clarius PA HD3 handheld ultrasound scanner.
LV function can be estimated based on the EPSS measurement, or the Clarius app will display an ejection fraction on the image screen
Note that conditions like atrial fibrillation, septal hypertrophy, and wall motion abnormalities can limit the accuracy of the EPSS measurement.
Axial Contraction/ Fractional Shortening
The third tool to assess how well the left ventricle is contracting is to look at axial contraction. This is done by imaging perpendicular to the long axis of the ventricle from the parasternal window. During contraction, the muscle in a normal heart gets much thicker and the LV diameter or distance in the axial plane shortens.
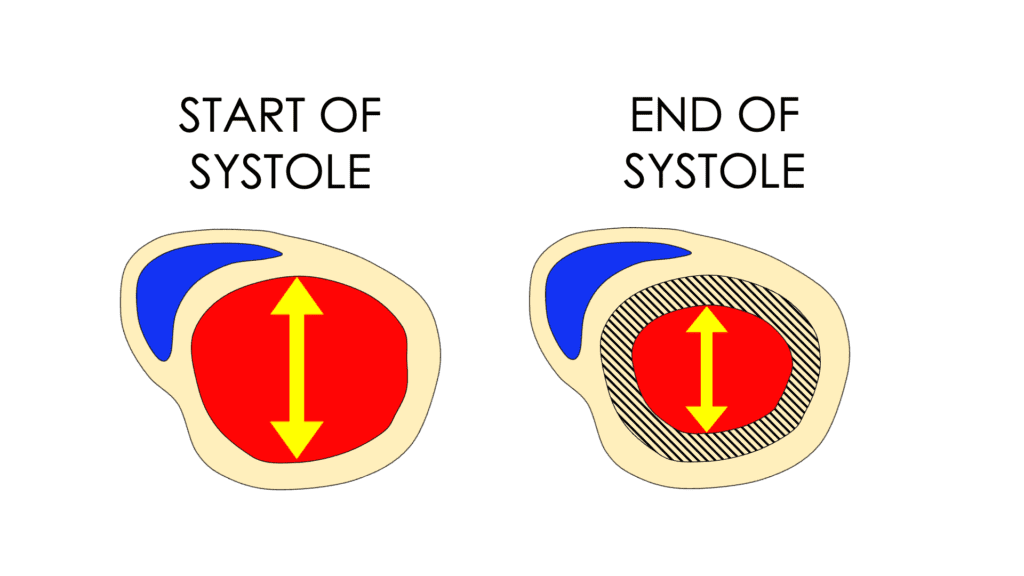
Two measurements and a simple equation are needed to calculate fractional shortening, and the easiest way to do this is using m-mode, with the cursor placed just on the apical side of the mitral leaflet tips. Measure the LV at its largest diameter for diastole, and when it’s the smallest for systole.
Learn how to measure FS in this video
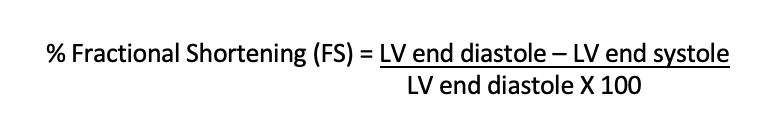
Normal range is 25 – 45%, which is different from the normal range for EF, which is 55 – 65%.
Longitudinal Contraction/MAPSE
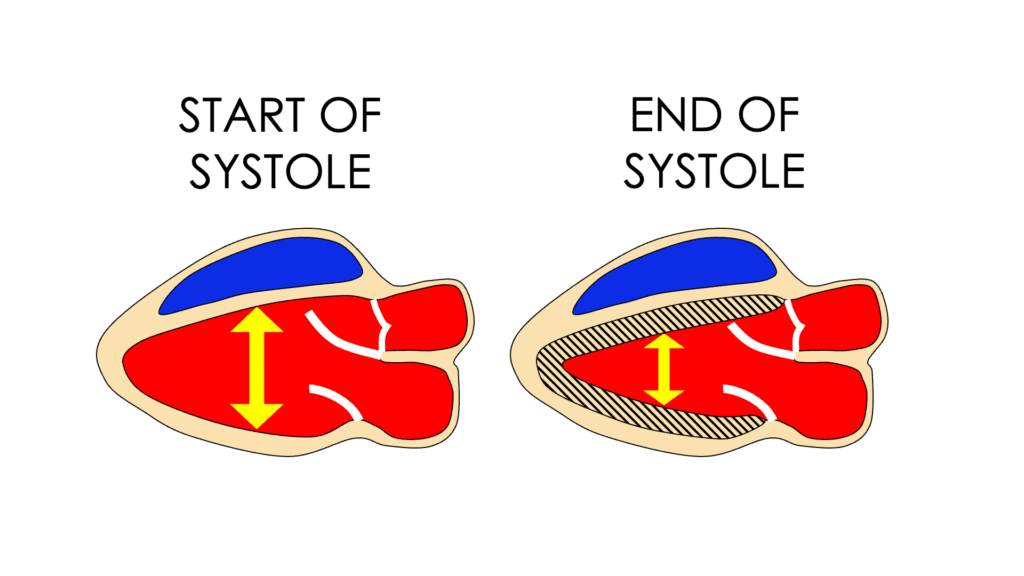
When imaging the heart in the long axis (from the apex), it is again evident that during contraction, the muscle thickens, and the chamber gets shorter. The LV apex doesn’t move, and the base of the heart moves toward the apex.
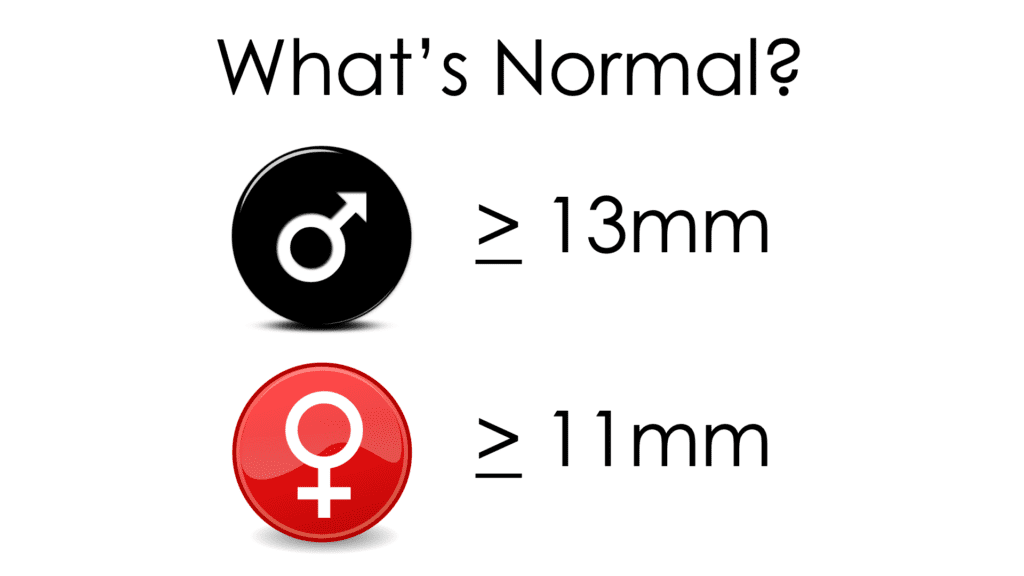
This movement can be quantified using a tool called MASPE, and it only requires one measurement. MAPSE is an acronym for Mitral Annular Plane Systolic Excursion, and is very easy to perform:
- Acquire an apical 4 chamber view on the heart,
- Place the m-mode cursor over the echogenic lateral mitral valva annulus,
- Freeze the m-mode and measure the movement of the annulus.
Dr. Cook shows how to measure MAPSE in this video using the Clarius PA HD3 handheld ultrasound scanner.
Dr. Cook stresses that all these tools are essentially linear measurements to describe a 3D structure, so it’s important to also visually assess the heart, keeping clinical scenario and patient history in mind. During the webinar he provides several great video examples and assessments that include the tools previously discussed.
Circling back to the original scenario of a patient who needed volume resuscitation but was in shock and hypotensive: he needed a quick bedside assessment of his heart prior to being given blood products. Two of the four tools discussed here indicate abnormal LV systolic function, therefore fluid resuscitation would likely cause volume overload and pulmonary edema. Based on these results, the treatment plan needed to be altered dramatically.
As with anything in life, you’ll get better with practice. You simply look at these hearts and start running those four tools through your head, and before you know it, you become quite a bit better at judging left ventricular function.”
About Dr. Tom Cook
Dr. Tom Cook is founder of 3rd Rock Ultrasound, an education company designed to help all healthcare providers integrate ultrasound into their practices. 3rd Rock Ultrasound offers a variety of accredited ultrasound courses throughout the year to empower emergency and critical care physicians with the ability to utilize POCUS to improve patient care.
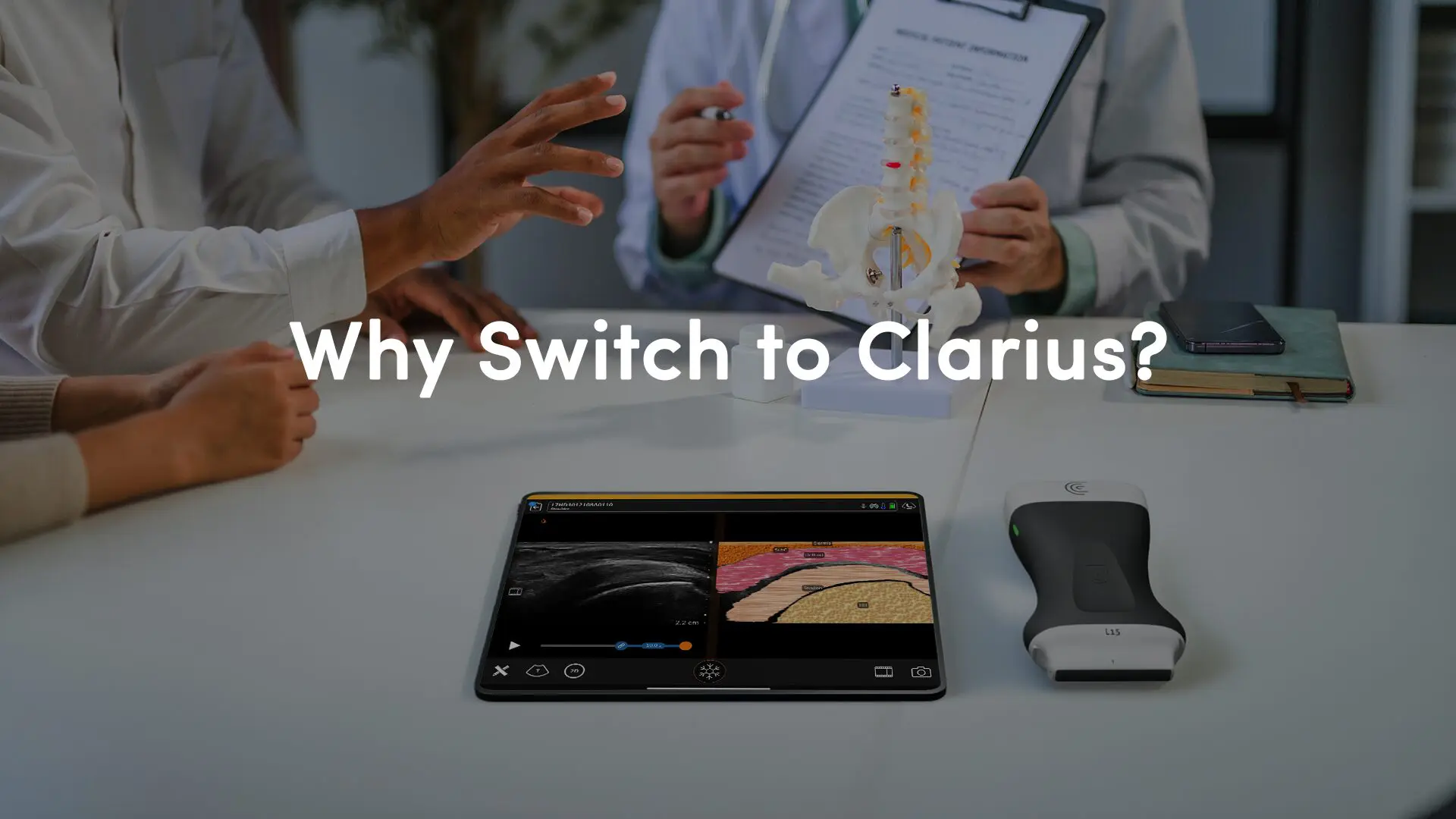
Get Answers Quickly in the ER with Clarius Handheld Ultrasound
Thanks to miniaturization and innovation with handheld ultrasound, you can now carry a high-definition ultrasound scanner in your pocket. To learn more about the high frequency Clarius PA HD3 handheld ultrasound scanner that Dr. Cook uses, visit our emergency medicine page where you be able to access webinars, see customer reviews and watch classroom videos. Feel free contact us today or request a virtual ultrasound demonstration at your convenience.