Daniel J. Kim, MD FRCPC
 | Dr. Kim is an emergency physician in Vancouver. To help Clarius users understand how they can use ultrasound in the screening and monitoring of COVID-19, we asked Dr. Kim to put together an article summarizing current best practices. Clarius will share updates on ultrasound use for COVID-19 as more information and resources are available. |
Since the outbreak of a novel coronavirus in Wuhan in December 2019 and its subsequent evolution to a pandemic in March 2020, there has been growing interest in the utility of lung ultrasound in the workup and management of COVID-19.
Screening
Given that imaging findings are nonspecific, in a clinically well patient with mild symptoms, there is no role for lung ultrasound. These patients should be tested with nasopharyngeal swabs for RT-PCR according to local public health guidelines.
There have been reports of cases of patients with typical chest CT findings of COVID-19 who had initial negative RT-PCR results. All 5 of these patients ultimately had positive RT-PCR results after repeated testing. Lung ultrasound may be helpful for patients with a high clinical suspicion of COVID-19 but negative RT-PCR screening if they demonstrate typical lung ultrasound findings for COVID-19. <1>
Technique
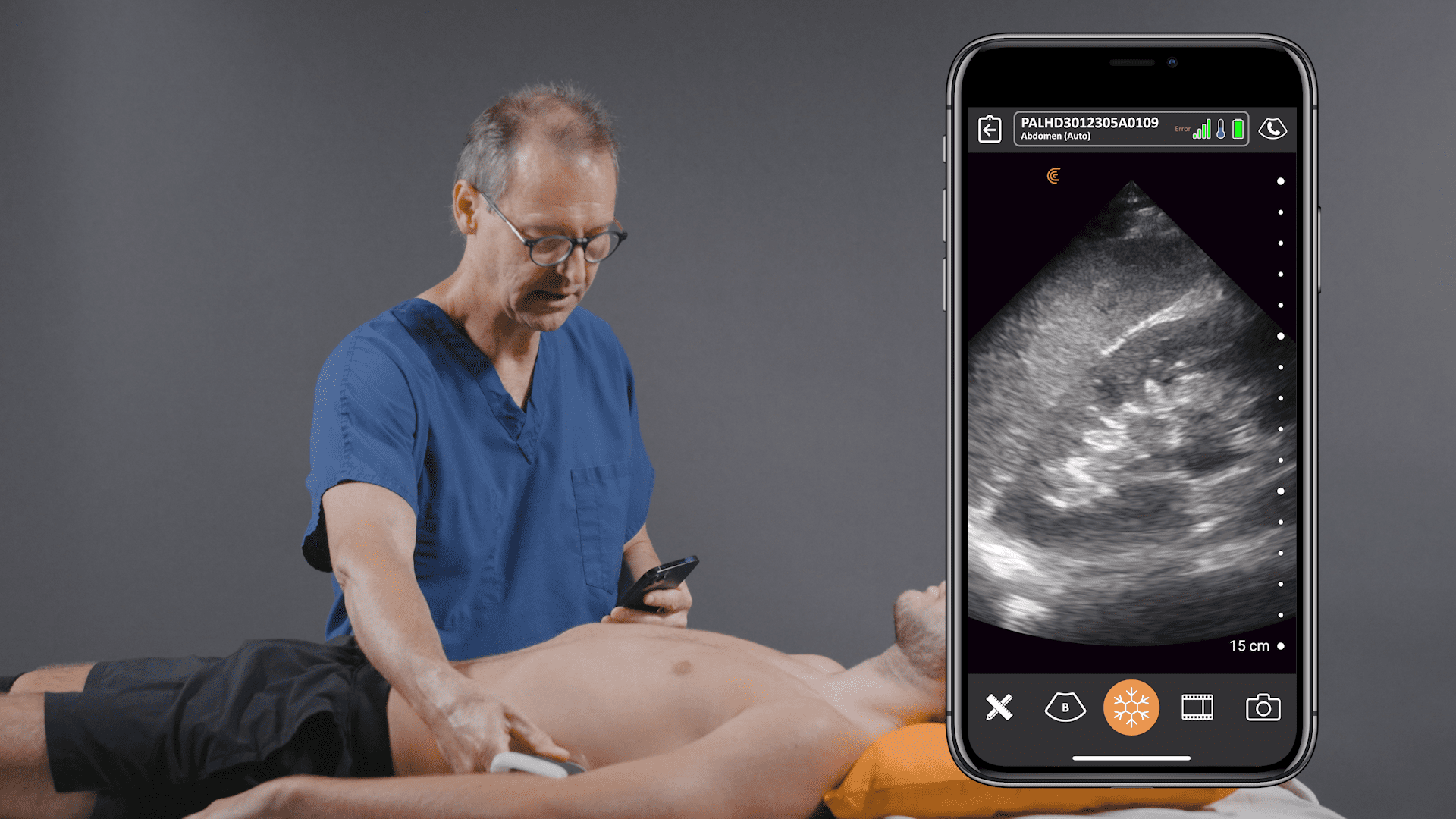
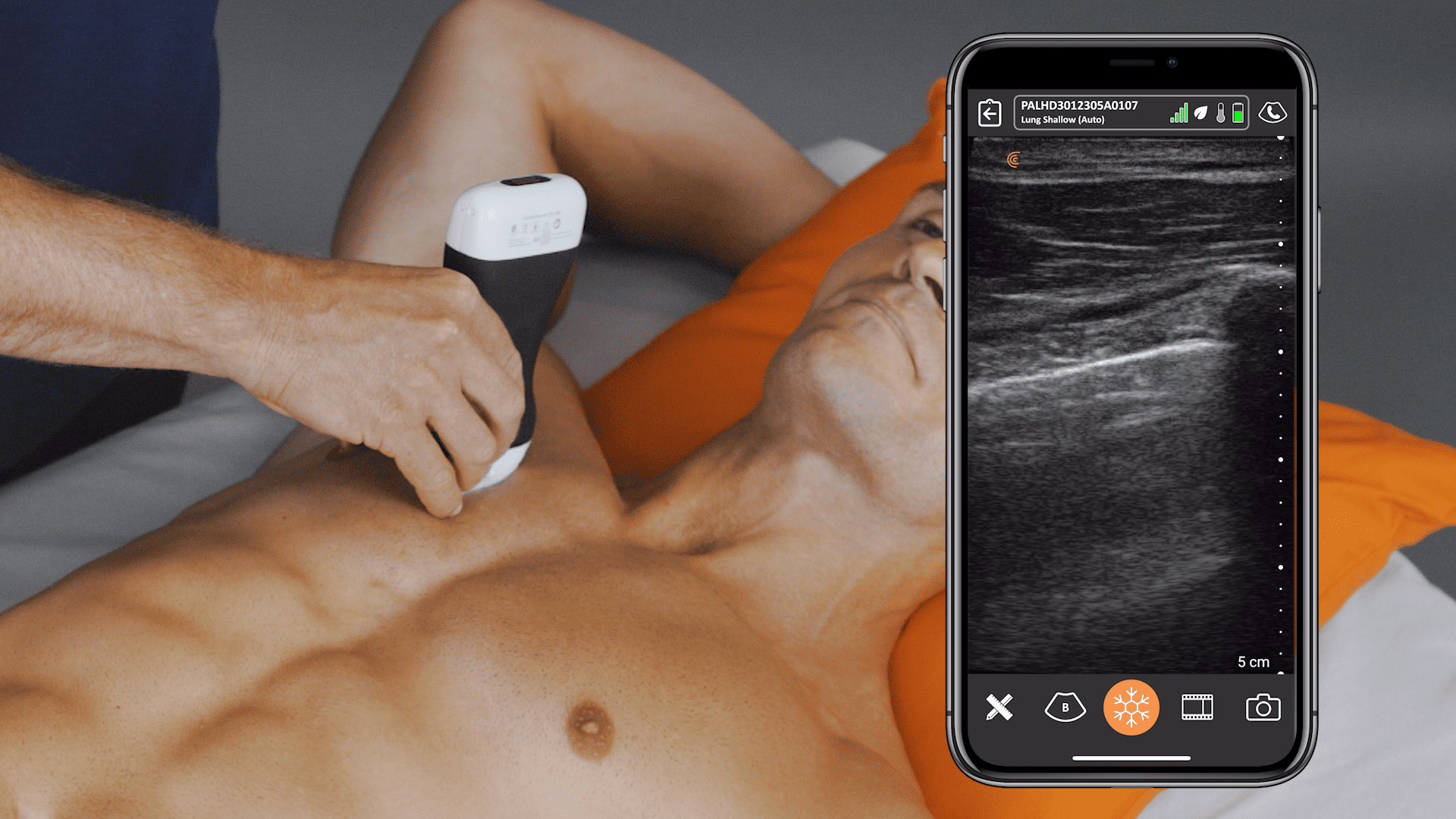
2 small studies describing COVID-19 lung ultrasound findings employed a focused 12-area approach. <2,3> Each lung was divided by the anterior axillary line and posterior axillary line into 3 areas: anterior, lateral, and posterior. Each of these areas was subsequently divided into an upper and lower field, so that each lung was divided into 6 areas. To maximize sensitivity, as much of the lung field should be visualized as possible.
Using a linear probe is preferable for identifying pleural and subpleural abnormalities. A curvilinear or phased array probe is better at demonstrating B lines. Lung scanning should be performed perpendicular to the contour of the pleural line.
Diagnosis
2 small studies including 20 patients each describe the following lung ultrasound findings in COVID-19: <2,3>
B lines with variable appearance, including focal, multifocal, and confluent
Subpleural consolidations
Larger consolidations with occasional air bronchograms
Pleural thickening and pleural line irregularity
A multi-lobar distribution of abnormalities is common. Ultrasound B lines correspond to the typical ground glass opacities visualized on CT imaging. Pleural effusions (other than small localized effusions) are rare. Abnormalities are most commonly visualized in the posterior and inferior lung fields.
In the early stages of infection, the main ultrasound finding is focal B lines. As the disease progresses, B lines can become multifocal and confluent, with further development into frank consolidations. A lines should reappear during convalescence.
The sensitivity and specificity of lung ultrasound for COVID-19 has not been determined. Specificity is likely low, given that B lines can be visualized in any disease process causing interstitial lung disease (for example, pulmonary edema, pneumonitis, viral pneumonia, pulmonary fibrosis, ARDS).
It has been suggested that for a patient with respiratory failure, a normal lung ultrasound should rule out COVID-19. Ultimately, lung ultrasound provides one additional datapoint to the full clinical picture.
Monitoring
A March 10th meeting document from the Gruppo Italiano per la Valutazione degli interventi in Terapia Intensiva (GIVITI) describes their current experience with COVID-19 in ICU patients. <4> From a monitoring standpoint, a diffuse B line pattern on lung ultrasound seems to respond well to PEEP. For patients with consolidation posterolaterally and inferiorly, pronation seems to be effective.
References
1. Xie X, Zhong Z, Zhao W, et al. Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RT-PCR Testing. Radiology 2020;200343. doi:10.1148/radiol.2020200343.
2. Huang Y, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19). SSRN 2020. doi:10.2139/ssrn.3544750.
3. Peng Q, Wang X, Zhang L. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med 2020. doi:10.1007/s00134-020-05996-6.
4. Gruppo italiano per la Valutazione degli interventi in Terapia Intensiva (GIVITI). COVID ITU Patients – Italian Experience. March 3, 2020. Available at: https://www.dropbox.com/s/r2ca63ckaimp1f6/COVID%20ITU%20Patients%20Italian%20Experience.docx?dl=0