Excerpt from an article that appeared first on Kidney News Online, written by By Nathaniel Reisinger MD
Improvised hastily by a young physician to avoid the embarrassment from direct auscultation of a particularly buxom patient’s chest, the stethoscope recently celebrated its 200th anniversary. After initial resistance, it has since become standard of care and a ubiquitous icon of the physician.
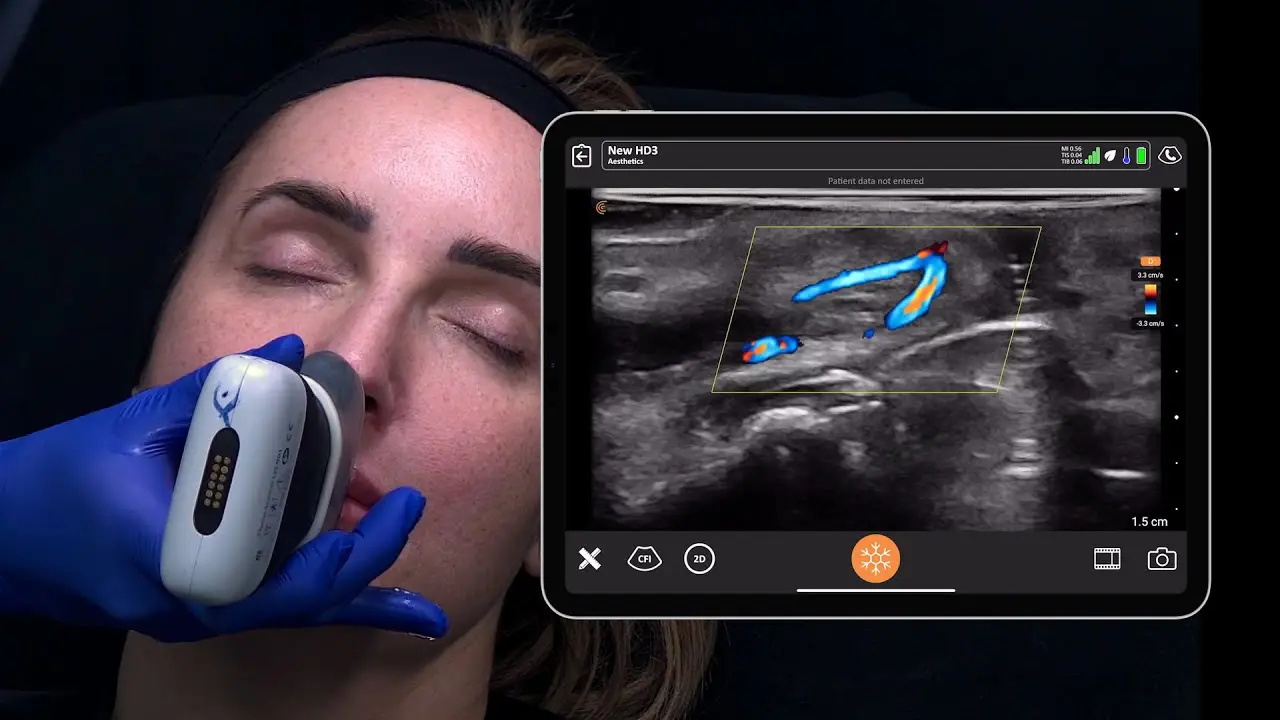
Technology has improved since the Napoleonic era, and more sophisticated devices are now available to augment the physical exam. Ultrasound was originally applied as sonar to hunt submarines in the First World War, but was quickly co-opted into the medical field. Early machines occupied entire rooms, but now powerful imaging devices are handheld and can be paired wirelessly with smartphones allowing ultrasound to be used on bedside rounds.
Point-of-care ultrasound (POCUS) has been used by obstetricians, cardiologists, and emergency medicine physicians for more than 20 years to answer focused questions and expedite clinical decision-making. In this time, POCUS has become increasingly incorporated into medical school curricula across the country. Some schools even provide point-of-care devices for all of their medical students; an entire generation of young physicians is training with concept of the ultrasound-stethoscope.
Nephrologists have not fallen behind in this trend. Many already use ultrasound for dialysis catheter placement and percutaneous kidney biopsy. Interventional nephrologists are using ultrasound to look at fistula stenoses and renal intensivists have taken it a step further, bringing a suite of simple ultrasound tests to the bedside to diagnose undifferentiated shock.
Nephrology fellows are already demanding formal training in ultrasound. It was true in 2008 and confirmed in a recent survey of fellows conducted in 2016. Whereas only 12% of fellows reported having formal ultrasound training, 44% wanted additional instruction in ultrasound interpretation.
To read the rest of the article, please click here.