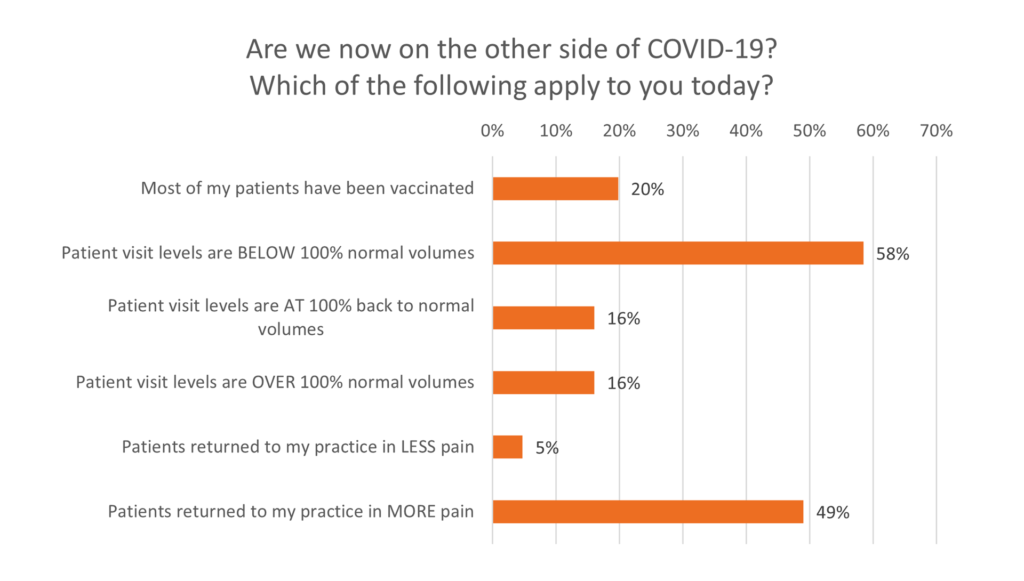
Over 100 pain management specialists reported on the continued impact of the pandemic in a recent poll conducted during the webinar, Practical Pandemic Pain Remedy, hosted by Clarius Mobile Health. Unsurprisingly, 64% of pain specialists confirmed a decrease in patient visits during the pandemic, while 54% said patients are suffering unnecessarily.
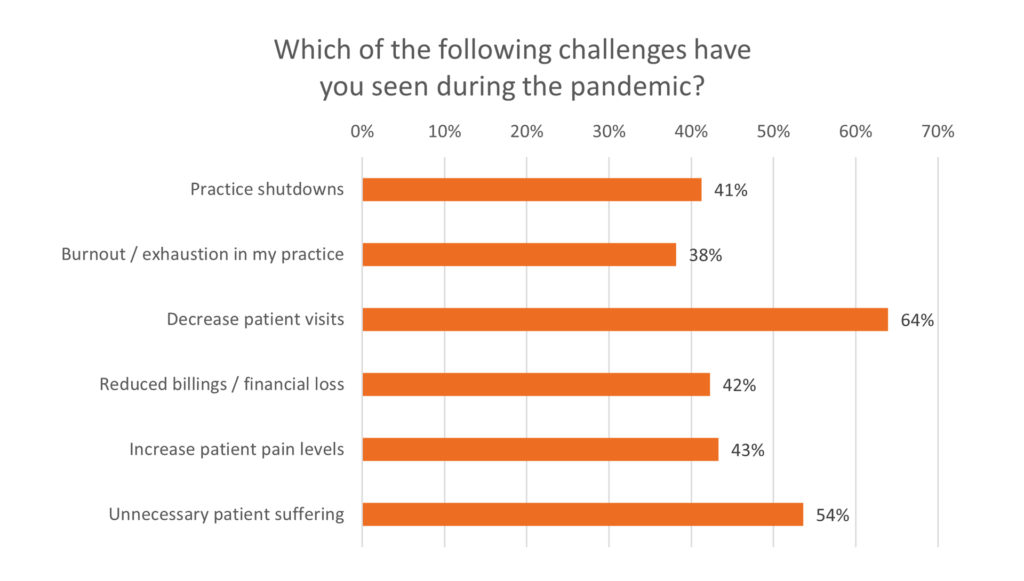
Our poll results on reduced patient visits mirror the results of a survey administered by the American Society of Pain Physicians last summer. The ASIPP data showed that over 90% of interventional pain practices have experienced a significant financial impact, as outpatient and elective interventional procedures have been reduced or interrupted to reduce the spread of COVID-19.
What we know from evidence-based risk mitigation is that chronic pain patients require continuity of care and this has been really hard to accomplish during the pandemic,” says emergency physician Dr. Oron Frenkel. “Unfortunately, there’s only so much intervention that can be accomplished with telemedicine, especially in pain management.”
While vaccinations are becoming more widely available in certain regions of the world, access in not yet ubiquitous. Only 20% of physicians polled reported that most of their patients have been vaccinated, leaving 80% of physicians with patients at risk of infection. The poll also confirmed a rise in patient suffering as they return for treatment. A significant 49% of physicians reported that patients are returning with more pain, while only 5% reporting less pain. Clearly, the negative impacts from COVID-19 on interventional pain management are not yet behind us.
Dr. David Rosenblum, Director of Pain Management at the Maimonides Medical Center in New York, managed to keep his practice open for many of his chronic pain patients. As he and his team successfully managed to navigate the challenges of practicing pain management during the pandemic, we invited him to share his learnings during a one-hour webinar, “Practical Pandemic Pain Remedy: Ultrasound-Guided Occipital, Erector Spinae & Tendon Sheath Injections.” Watch the webinar now or read on for some quick tips.
COVID-19 and Pain Management
This whole pandemic has definitely been quite crazy for all of us,” says Dr. Rosenblum. “With patients coming to the office, you want to first figure out what’s going on with the patient. Of course, you ask about symptoms, contacts, travel. You want to know if they had COVID, when did they recover, proof of the recovery.”
According to Dr. Rosenblum, guidelines for the types of medications to provide patients based on their vaccination status are evolving.
Last I checked, if you’re using dexamethasone, you want to wait about two weeks, methylprednisolone, usually four weeks. And then after you give the second dose, you want to wait at least two weeks until you give the steroid injection. But, of course, these are guidelines,” he adds. “If a patient is desperate and in bad shape, you may not follow these guidelines. You do what’s right for the patient, which of course is not always obvious, but you use your judgment. We’re not technicians, we’re physicians, and we need to weigh the good and the bad of everything we do.”
Pandemic Precautions in the Office
While disinfection is always a priority in clinics, COVID-19 has made it more important than ever. Patients are also temperature-screened and have their vitals checked before procedures at the Maimonides Medical Center. Whether or not a patient is required to provide results of a COVID test prior to a procedure depends on the type of procedure and where it takes place.
If you’re doing a procedure in an operating room or a Quad A certified room, you’ll probably need to get a COVID test if you’re within five days of that procedure,” Dr. Rosenblum explains. “If you’re doing a knee injection, for example, in a regular office room, you should not need that. Of course, guidelines may change, and it also depends where you’re practicing and at what stage of the pandemic you are. In New York, things are winding down a bit since most of our patients and physicians are vaccinated at this point.”
Watch the Webinar for Pro Tips on Treating Three Common Pain Conditions
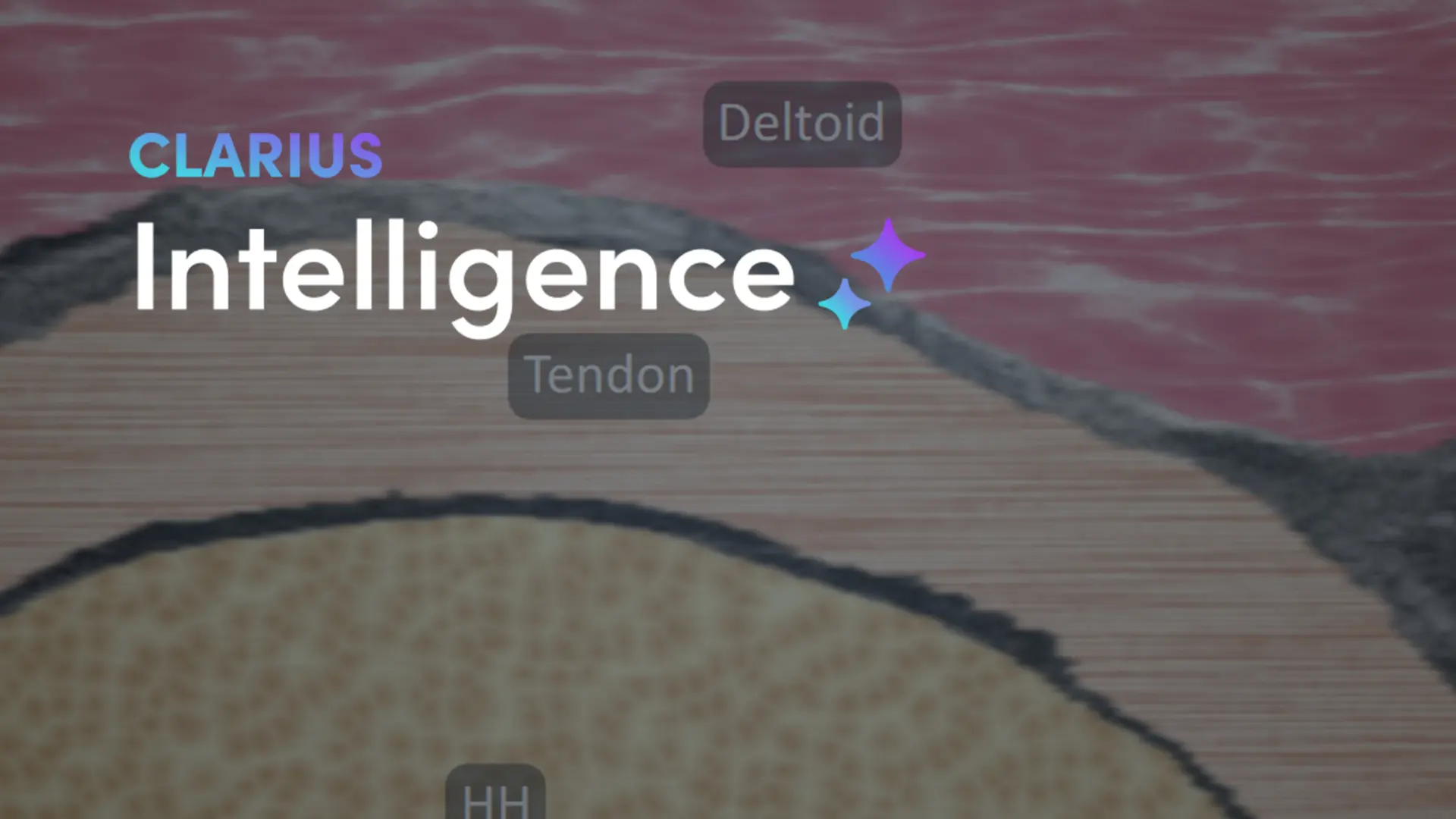
Dr. Rosenblum presented three real patient cases where he used ultra-sounded guided pain medicine injections to remedy pain worsened by the pandemic. Watch the webinar to see him in action with the Clarius L7 HD high frequency wireless ultrasound scanner. Or watch his new Clarius Classroom video tutorials on how to use ultrasound guidance to safely perform an erector spinae block, an occipital nerve block and a gluteal tendon injection.
A prolific educator, Dr. Rosenblum hosts the Pain Exam Podcast and created a Pain Exam Board Review, which has helped over 3,000 pain management physicians become board certified.
To learn more about how Clarius HD is used to guide injections, visit our wireless ultrasound for pain management page. Or contact us to today to book a demo with one of our ultrasound experts.