In the practice of plastic surgery, ultrasound has progressed from an experimental novelty for some to an essential tool for safety and precision for many clinicians. While traditional palpation has long been the standard for assessing the abdominal wall, recent studies indicate that relying purely on touch can be misleading, particularly regarding semilunar lines and oblique borders.
During a recent Clarius webinar, Dr. Khanh Nguyen, a plastic and reconstructive surgeon specializing in body contouring, shared his expertise on using high-frequency ultrasound to revolutionize the diagnosis and management of Diastasis Recti (DR). The webinar is now available to watch at your convenience.
In the meantime, below are the key takeaways for surgeons looking to integrate Point-of-Care Ultrasound (POCUS) into their practice.
1. Redefining Abdominal Anatomy for Better Outcomes
Understanding the nuances of the superficial fascia is critical for lipo-sculpting. While classic texts describe two layers (Camper’s and Scarpa’s), Dr. Khanh notes that below the umbilicus, modern anatomical studies reveal three distinct layers:
- Superficial Adipose Tissue: The variable layer where most fat deposits reside.
- Scarpa’s Fascia: A thin but strong membranous layer crucial for closing dead space and reducing tension during abdominoplasty.
- Deep Adipose Tissue: A layer often close to the muscle containing the lymphatics.
Clinical Pearl: Dr. Khanh advises preserving the deep adipose tissue during abdominoplasty. This layer houses the lymphatics; preserving it significantly reduces postoperative drainage and the risk of seroma.
Video: Abdominal Wall Ultrasound Assessment for Body Contouring
In this video, Dr. Khanh performs an ultrasound assessment of a patient’s abdominal wall to enhance his surgical planning.
2. Diastasis Recti: Beyond the Physical Exam
Dr. Khanh defines DR as a linea alba width of more than 2.2 cm at 3 cm above the umbilicus. However, the location of the separation matters as much as the width.
The “Hidden” Upper Separation
One of the most compelling cases presented involved a patient who had previously undergone a “mini-tuck” yet remained unhappy with a protruding upper abdomen.
- The Misdiagnosis: The previous surgery addressed the lower abdomen but ignored the upper midline.
- The Ultrasound Find: Ultrasound revealed a large gap (3.2 cm) extending from the xiphoid process, which was missed during the initial procedure.
- The Lesson: Upper separation is the most common subtype of DR. Repairing only the lower abdomen can actually worsen the upper separation.
VIDEO: Ultrasound Assessment of Diastasis Recti
Dr. Khanh demonstrates his technique for assessing diastasis recti using ultrasound to evaluate the muscles and fat layers of the abdominal wall for diagnosis and pre-surgical planning. Watch this video to learn how to perform a detailed assessment with the Clarius L15 HD3 high-frequency linear scanner.
3. Preoperative Safety: Screening Bariatric Patients
For patients who have undergone massive weight loss or laparoscopic procedures, ultrasound is a non-negotiable safety tool.
- Port-Site Hernias: Studies suggest the prevalence of port-site hernias in bariatric patients can be as high as 34%. Ultrasound allows you to measure the hernia neck; if it is wider than 2 cm, you may need to prepare mesh for the repair rather than a primary closure.
- Vascular Mapping: In patients with extreme skin laxity and deflation, major vessels may be more superficial than expected. Dr. Khanh shared a startling case where a patient’s aorta was only 1 cm beneath the skin.
- Actionable Step: Use ultrasound to map large vessels and apply targeted tumescent fluid to induce vasoconstriction, minimizing intraoperative bleeding.
Webinar Q&A: Addressing Surgeon Concerns
Dr. Khanh responded to questions from the live audience following his webinar presentation. The following are some highlights.
Q: Does using ultrasound add too much time to patient consultations?
“No, actually the contrary… It helps me save time because the patients and I can communicate a lot better.” Showing a patient their anatomy live—explaining that their bulge is visceral fat or muscle separation rather than just subcutaneous fat—streamlines decision-making.
Q: Is ultrasound accurate enough for measurements, or do I need an MRI?
Dr. Khanh is very confident in ultrasound measurements. He typically only orders an MRI for complex secondary (redo) cases or if the separation is unusually severe. For standard cases, ultrasound is sufficient.
Q: Do you need an endoscope to repair the diastasis?
Not always. For a full abdominoplasty (open approach), an endoscope is not needed. However, for patients requesting a “scarless” or mini-incision approach, the endoscope is valuable for determining the extent of plication required.
Click here to watch the full webinar.
Why Clarius is a Popular Choice for Plastic Surgeons Using Handheld Ultrasound
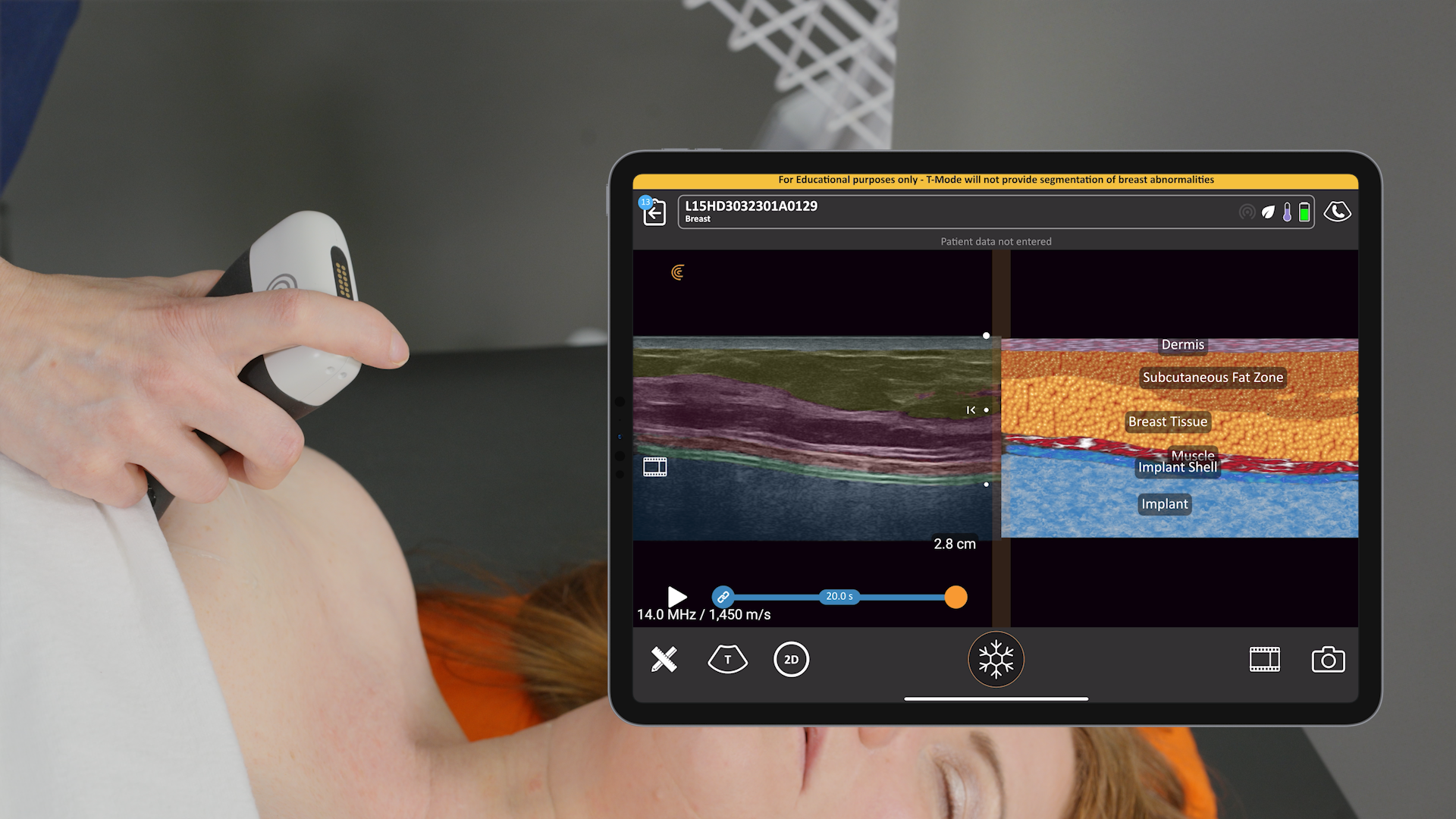
During the webinar, Sonographer Janaye Smith performed a live demonstration showcasing the Clarius L15 HD3, a high-frequency wireless scanner designed for superficial imaging. Here are the top reasons why plastic surgeons, including Dr. Khanh choose it for their practices:
- Wireless & Zero Footprint: The system is handheld and connects to iOS or Android devices, eliminating bulky carts in the OR and making it easy to sterilize.
- High-Definition Imaging: It offers image quality that rivals traditional systems at a fraction of the cost (roughly 85% savings).
- T-Mode: A game-changer for education and training. This AI-powered feature provides a split-screen view, overlaying a graphical representation of skin, fat, and muscle layers alongside the grayscale image to help surgeons instantly identify anatomy.
- Heat Management: The new “Cool Power Fan” allows for extended scanning periods without the device overheating—crucial for complex mapping or teaching.
Ready to elevate your practice?
Ultrasound is no longer just for radiologists. As Dr. Khanh states, “If we have precision, we will have better surgical outcomes”.
Learn more about Clarius ultrasound for plastic surgery. We would be delighted to provide a personalized virtual demonstration at your convenience.