In veterinary medicine, trauma cases are a common sight in urban emergency rooms, making up 11% to 13% of all cases. When a canine patient presents with blunt trauma, such as being hit by a car, it’s crucial to quickly identify and address life-threatening injuries. While blunt abdominal injuries account for a significant portion of trauma cases (~45%), thoracic injuries occur in about 50% of these patients, making them a primary concern.
According to Dr. Soren Boysen, DVM, DACVECC, a professor of small animal emergency and critical care at the University of Calgary, a patient that is “unstable” from a respiratory standpoint and has a high heart rate could be “cardiovascularly unstable”. Dr. Serge Chalhoub, DVM, DACVIM (SAIM), an associate professor of internal medicine also at the University of Calgary, agrees, adding that such patients may also be in pain and anxious, working against efforts to help them.
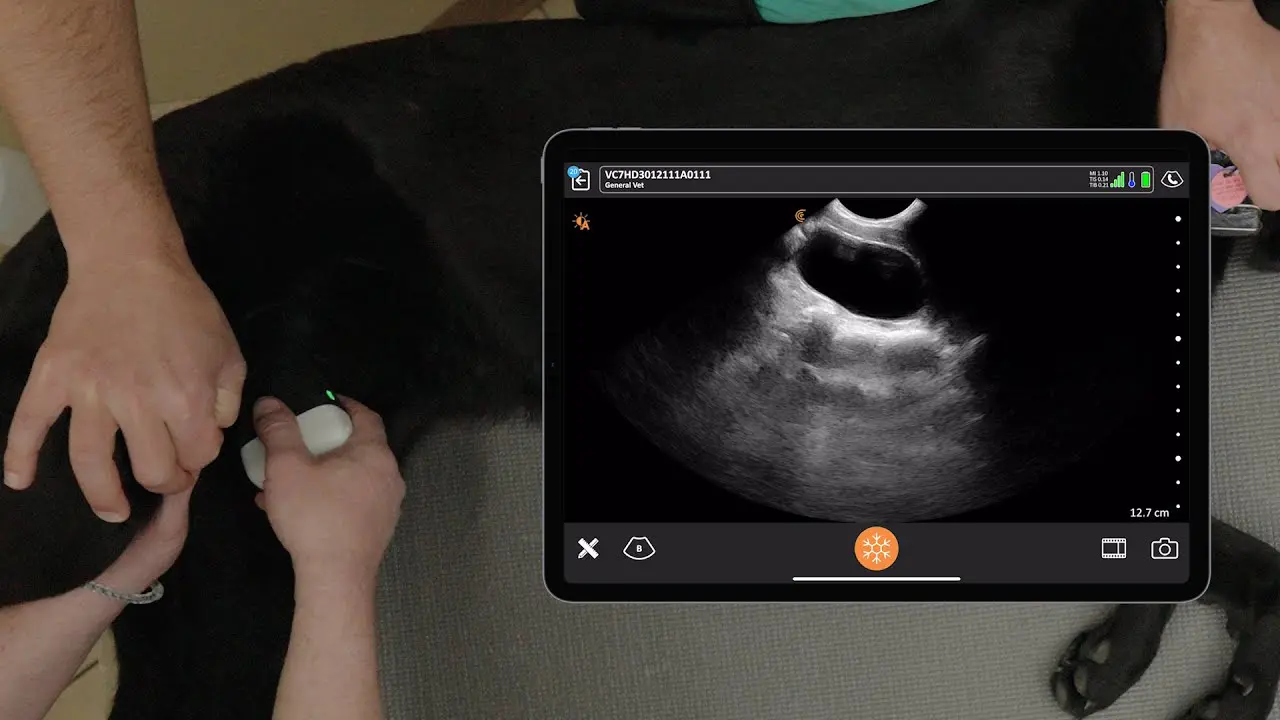
Dr. Boysen and Chalhoub are strong advocates for using point-of-care ultrasound (POCUS) for emergency triage and management of these patients. Their approach is patient-centered and targeted, focusing on the most life-threatening issues first, such as respiratory distress or internal bleeding. Unlike a full physical exam, POCUS is an abbreviated assessment that provides critical information quickly, allowing for immediate intervention.
During a one-hour Clarius webinar focused on canine trauma that is now available on-demand, Dr. Boysen and Chalhoub explore the applications of POCUS to detect potential thoracic injuries and provide valuable diagnostic information beyond the physical exam. Watch the webinar at your convenience and read on for some key takeaways.
Common Thoracic Injuries and POCUS Findings
Dog versus car usually doesn’t bode well for the dog and a patient often presents with respiratory distress and an unstable cardiovascular status. POCUS is highly effective for diagnosing common thoracic pathologies. Here’s what to look for:
Pulmonary Contusions: These are the most frequent thoracic injury in blunt trauma patients, with an incidence of 58%. On ultrasound, they appear as an increase in B-lines and/or lung consolidation. B-lines are vertical white lines that originate from the pleural line, move in sync with lung sliding, and extend to the far field, often obliterating A-lines. The presence of B-lines at a probe location rules out pneumothorax at that site. The sudden disappearance of B-lines as you scan caudally can be a clue to the presence of a pneumothorax.
Pneumothorax: Occurring in about 47% of trauma patients, a pneumothorax is a pocket of air between the chest wall and the lung. Ultrasound is much more sensitive than thoracic radiography for detecting small pneumothoraxes. A pneumothorax is ruled out if you observe lung sliding or B-lines. The definitive “rule-in” signs for a pneumothorax are the lung point and an abnormal curtain sign. The abnormal curtain sign can be a “double curtain sign,” where soft tissue appears to break into a region of pneumothorax and then disappear, or an “asynchronous curtain sign,” where the lung and other tissues move in opposite directions during respiration. According to Dr. Boysen, he now diagnoses the majority of pneumothoraxes from an abnormal curtain sign because he finds it easier to assess than lung sliding.
Watch the webinar for examples of the curtain sign in ultrasound. You can see Drs. Soren Boysen and Serge Chalhoub demonstrate their pleural space and lung ultrasound technique in this 11-minute video.
Hemothorax and Diaphragmatic Hernias: Hemothorax (blood in the chest cavity) is less common, found in about 18% of cases, and often involves low-volume bleeds since life-threatening arterial tears typically don’t allow patients to survive long enough to reach a clinic. Hemothorax is identified by anechoic fluid separating the chest wall and the lung. Diaphragmatic hernias are seen in approximately 6% of trauma patients and are often associated with blunt abdominal trauma. They can be diagnosed with ultrasound by visualizing abdominal organs, such as the liver, cranial to the diaphragm.
In this 4-minute video, Dr. Boysen demonstrates how to perform a thorough 5 point abdominal ultrasound exam in under a minute.
Rib Fractures: The incidence of rib fractures in trauma patients is about 14%. While historically diagnosed with radiographs, a study showed that ultrasound can be as sensitive as a board-certified radiologist interpreting radiographs for diagnosing rib fractures. A normal rib appears as a smooth white line in a long-axis view. A rib fracture is diagnosed by observing a discontinuity or “step” in the cortex of the rib.
Key Clinical Takeaways
- Triage First, Scan Second: The first step is to assess if the patient is stable or unstable. If they are unstable, the goal of POCUS is to quickly identify and address the most immediate life-threatening problem. As Dr. Boysen said, “We’re going to put a point of care ultrasound evaluation. We’re going to use that to assess this patient”.
- A “Black and White” Decision: In a patient with respiratory distress and potential bleeding, start with the most life-threatening problem. While some clinicians may choose to start with the abdomen, a patient with significant respiratory distress will likely benefit most from a rapid thoracic assessment.
- Protocol-Free Scanning: Use sonographic landmarks rather than memorized rib-counting protocols. Air rises, so in a sternal or standing patient, the most sensitive location to check for a pneumothorax is the most caudal dorsal site. By finding the cranial border and then the caudal border (the curtain sign) and sliding dorsally, you can systematically scan the thorax.
- The Curtain Sign is Key: An abnormal curtain sign, such as the “double curtain sign” or “asynchronous curtain sign,” is a strong indicator of a pneumothorax and a compelling reason to perform a thoracocentesis.
- POCUS for Treatment and Monitoring: POCUS can be used to guide procedures like thoracocentesis, improving safety and reducing complications. It also allows for serial exams to track the progression or resolution of pathologies over time, such as fluid accumulation or pulmonary contusions.
Q&A from the Webinar
Do you ever do dynamic scanning to make sure the double curtain goes away or gets smaller?
After a thoracocentesis, you can use ultrasound to re-evaluate the patient by looking for the lung point and the curtain sign. The goal is to see the lung point move dorsally and the double curtain sign resolve and become a normal curtain sign.
What Medication are you using to before scanning patients?
Opioids like methadone (0.2-0.4 mg/kg) or fentanyl are often used for analgesia and anxiolysis in trauma patients. Opioids are preferred in the emergency setting because they are fairly respiratory and cardio-sparing and can be reversed if necessary.
How do you position patients for scanning?
POCUS exams should be performed with the patient in a position of maximal comfort, such as sternal or standing. The principles remain the same regardless of patient position—air rises, so you should always scan the most non-gravity-dependent region to check for pneumothorax. Rigid, memorized protocols that ignore patient positioning can lead to missed diagnoses.
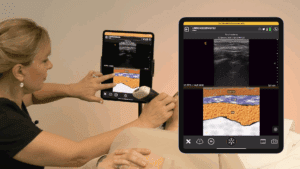
Why Clarius is a Popular Choice for Veterinary Practices
Clarius HD3 vet scanners are designed to deliver high-definition, wireless ultrasound imaging with the performance of a traditional system at a fraction of the cost. The wireless design and zero footprint make them highly portable, enabling clinicians to perform exams anywhere in the clinic or in the field without wires getting in the way or startling animals. The HD3 vet scanners, including the C7V microconvex, which is used for small animals like dogs and cats, come with an intuitive, AI-powered app for iOS or Android devices that streamlines workflows and automatically optimizes imaging. The Clarius ecosystem includes access to Clarius Cloud for unlimited exam storage and management, Clarius Classroom videos, and a one-click telemedicine feature with Clarius Live, making it a comprehensive and user-friendly solution for veterinary professionals.
To learn more about how you can add wireless ultrasound to your practice, visit our Veterinary Specialty Page. There you’ll have access to additional webinars and classroom videos.
To find out which scanner is best for your practice, request a personalized virtual ultrasound demo.