By Marc Salzman, MD, FACS
I knew nothing about using ultrasound when I started in 2012 with a laptop system. Now, I use ultrasound every day for various applications because using ultrasound helps me provide better patient care.
For those of you who are considering ultrasound for your practice, here are my 10 reasons why I think it’s the best new technology for cosmetic surgery since laser resurfacing in the 1990s.
1. Make a diagnosis with confidence in just one patient visit.
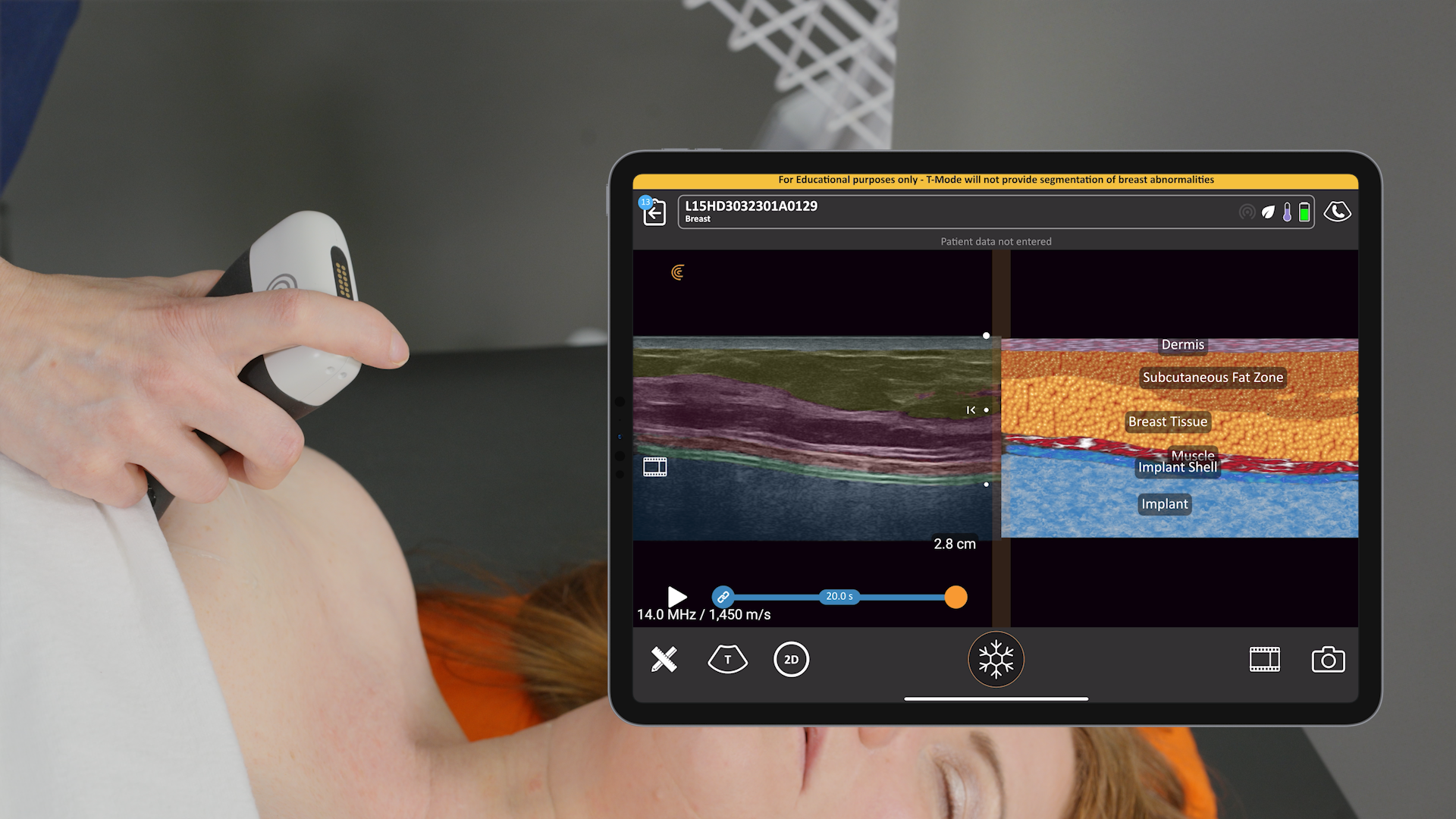
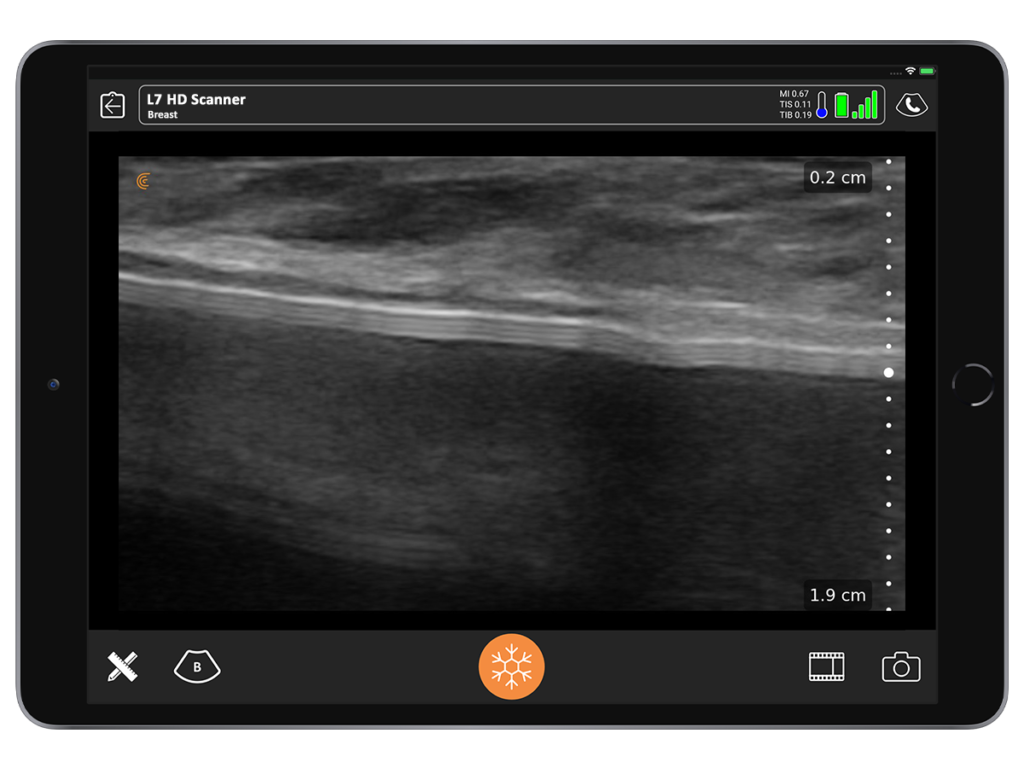
I use ultrasound for many applications in my practice. For breast, it enables me to make the diagnosis in just one patient visit. By looking under the skin, I can quickly answer several questions without sending the patient to a radiologist.
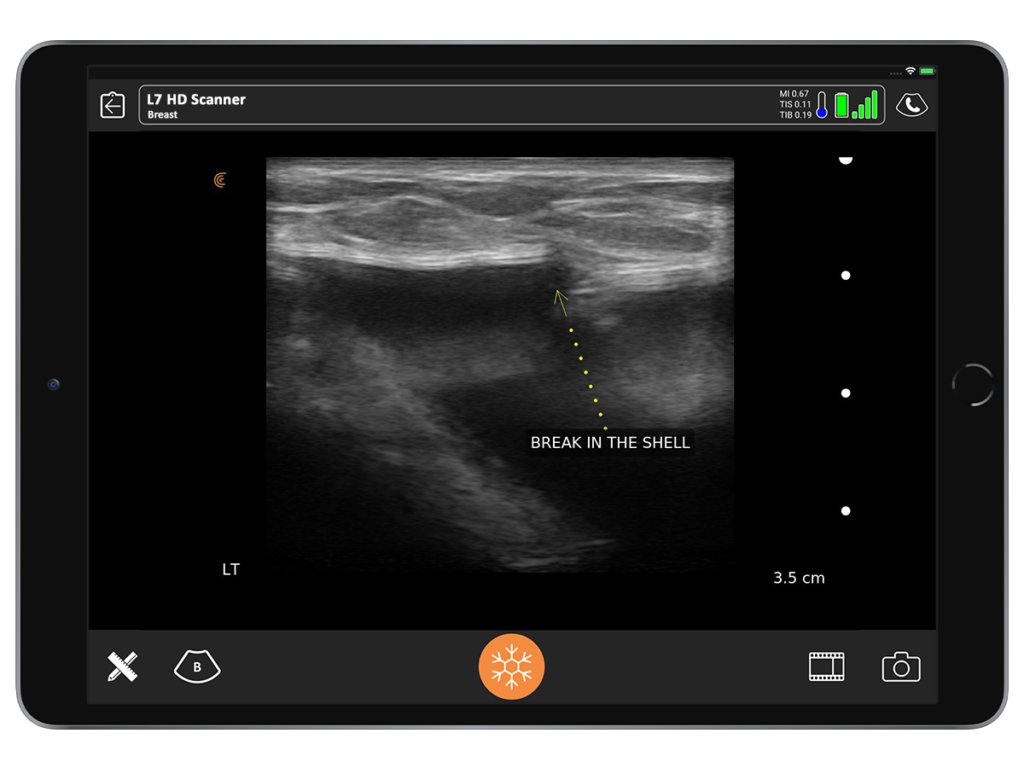
If an aspiration is needed, for example, I can do it in the office instead of waiting for someone else to do it. By using ultrasound, I’m able to say with a good degree of certainty whether an implant is broken or not. I’ve never seen a false negative.

2. Save time and money with a handheld ultrasound.
Using ultrasound in the office is quicker for the patient and it’s much more definitive. I quickly know what I’m going to do and I can tell the patient what the costs are going to be. For us, being able to accurately bill a patient has really made a big difference.
If we go to surgery and find a broken implant that we didn’t know about, all of a sudden, we’re doing a capsulectomy the patient wasn’t prepared for. The costs are going to be greater. The OR time is going to be greater. Which means, we likely lose money because it’s challenging to charge the patient who went in for an hour-long procedure, which ended up taking 3.5 hours.
A patient also isn’t happy to hear that she will have to wait for a diagnosis, make an appointment with another physician in a different location, and pay $1500 to $2500 for an MRI. Having ultrasound available at every appointment saves time and money for both the patient and my team.
3. Perform on the spot ALCL work ups with real-time imaging.
ALCL has really changed the dynamics of how we work up our patients. We commonly see patients who had an implant done 20 years ago. They have no idea if the implant is saline or gel or if it’s textured or smooth.
Being able to do the ALCL workup with ultrasound in the office gives us information to consider a lot of options. Are we taking the capsule out? Do we switch for a smooth implant? If it’s a textured implant, do we remove the implant altogether?
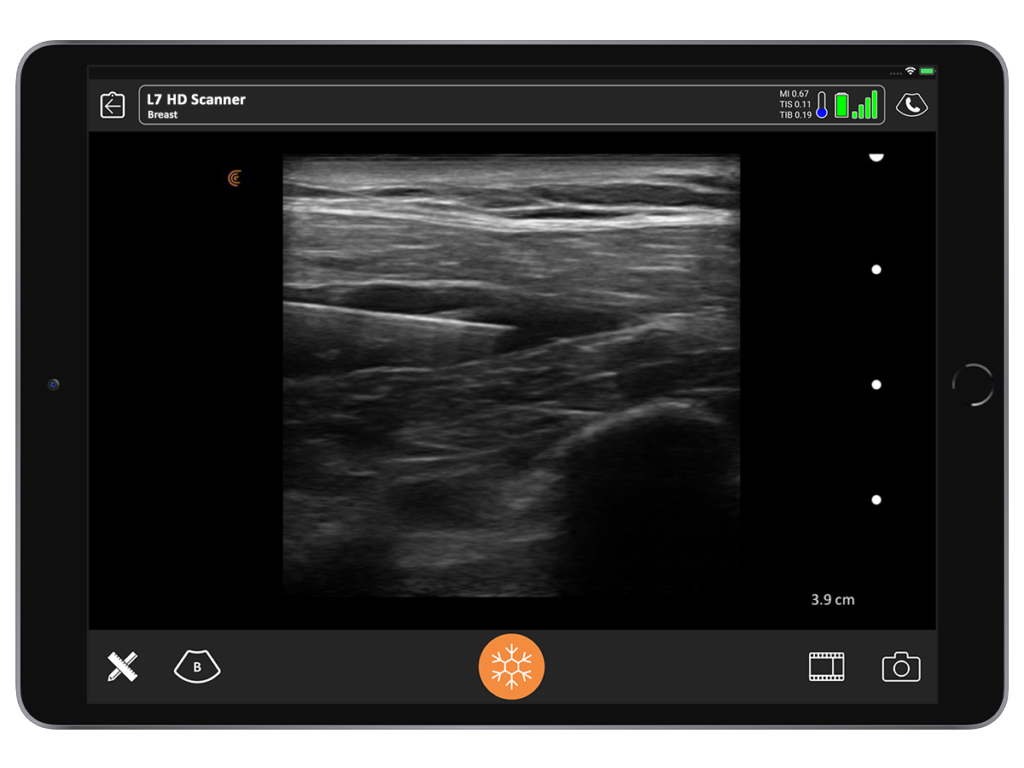
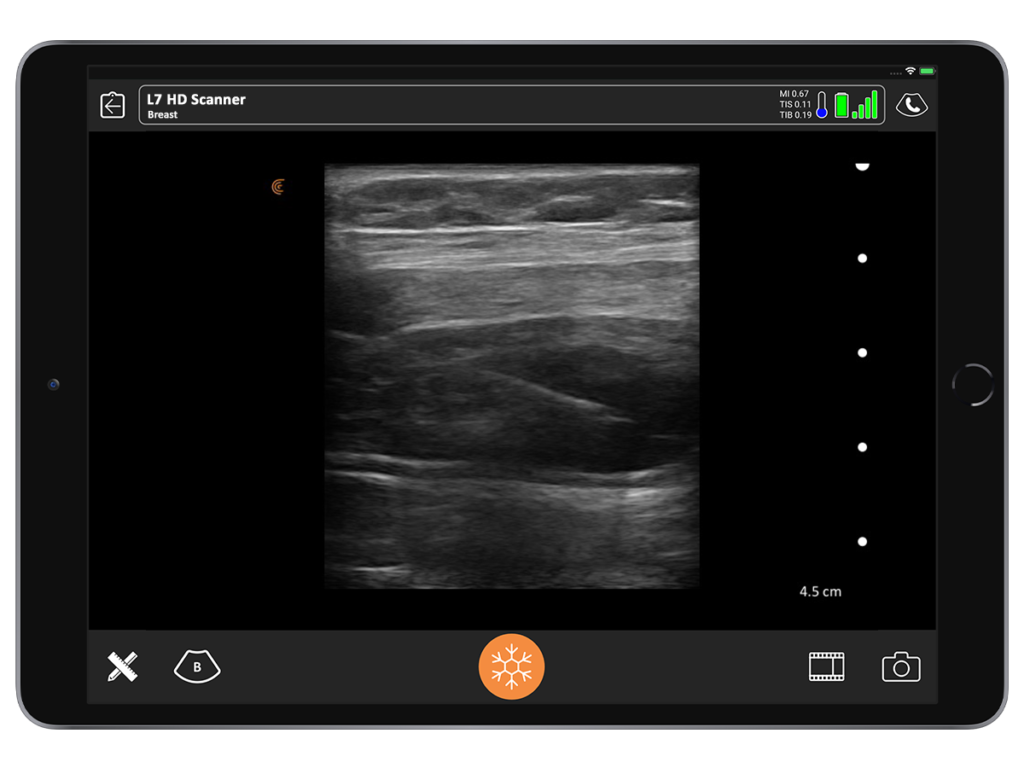
With ultrasound, you can tell a saline implant from a gel implant. You’re also able to differentiate between a textured versus a smooth implant. It’s also very easy to see a seroma. So, if you detect a smooth implant and the absence of seroma, you can tell your patient she’s unlikely to have ALCL.
For patients who come in with asymptomatic seromas, we are able to aspirate under ultrasound guidance in the office and send the sample to a pathologist for immunohistochemistry to check for CD30 markers.
4. Eliminate surprises in the OR, improving patient safety.
I have seen zero surprises in the operating room since I started using ultrasound to screen patients before cosmetic surgery.
I have never encountered a broken breast implant that I didn’t know about. I’m therefore always prepared with the right replacement implant during surgery.
By knowing what I’m going to see in advance, my surgeries are always on schedule and I never have to spend more time than I expected in the operating room.
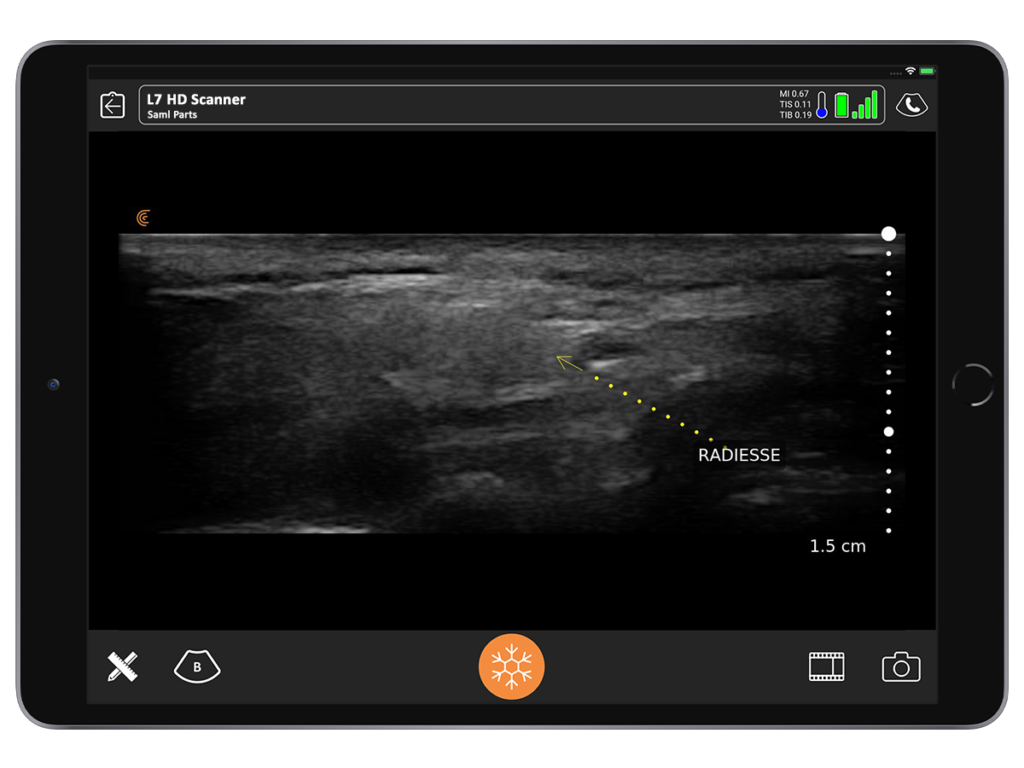
5. Ensure greater success with face filler procedures.
Sometimes I encounter deep nodules that patients say they can feel, but I can barely feel. A nodule may been caused by an injection with calcium hydroxyapatite that was given a year ago or longer. With ultrasound, we can see the nodule and perform a direct triamcinolone injection to ensure it goes directly into the little nodule.
Although I haven’t personally encountered this issue, in theory, it is possible to have a hyaluronic acid occlusion of a vessel from a thrombotic inclusion. Under direct visualization with ultrasound doppler, you can put the hyaluronidase very close to the vessel and bathe it in the hyaluronidase and do it every 10 minutes to clear it.
You’re much more likely to have a better outcome using ultrasound guidance because you can more accurately place the hyaluronic acid into the offending area and near the vessel that’s compromised.
6. Improve patient confidence and peace of mind.
I often see patients who have been in an accident and feel that something has changed with their implant. It looks and feels different to them and they are concerned that it may be broken.
By performing a quick scan during the consult, I give them immediate peace of mind by confirming with confidence that the implant is not broken.
7. Reduce pain with nerve blocks.
For nearly 3 years now, I’ve been helping patients recover more quickly and comfortably following mommy makeovers using nerve blocks.
A LAP (lateral approach pectoralis) block is a very simple procedure under ultrasound guidance. We place a long-acting Marcaine-like substance (Ropivacaine), which is the L-isomer of Marcaine, just under the lateral board of the pectoralis and infiltrating towards the thoraco-acromial artery. It’s a little safer and less cardio toxic than Marcaine.
The block lasts about 8 to 10 hours. We start by placing a small test dose once we pass the ultrasound-directed needle between the pectoralis major and minor to see the anechoic spread with the medication between the two muscles. Then we put 15 ccs of Ropivacaine per side.
With this block, I have observed my patients reduce their time in the PACU down to less than 15 to 20 minutes. We don’t see complications such as a high riding implants that are way up in the underarm necessitating massage protocols or necessitating fancy bras or straps. Patients aren’t susceptible to direct spasms, because when you’re blocking from lateral to medial, you’re getting the branches at the medial and lateral pectoral nerves, so the muscle is almost flaccid.
Patients are more comfortable. In addition to spending less time in the PACU, they have less narcotic use and so less nausea and vomiting. I’ve heard from patients who go out to dinner the night of the procedure thanks to this block. It has been wonderful!
For tummy tucks, the TAP block has revolutionized pain control. We’ve become proficient at placing long-acting blocks that lasts for three days. Patients are up and moving sooner. Their downtime has gone from 10 to 14 days to 6 to 8 days.
Exparel, which is the long acting numbing medicine we use, has really made a fantastic contribution to earlier patient recovery. Since we don’t get good coverage up high above the umbilicus from a TAP block (without risking paralyzing the diaphragm), we just directly infiltrate some Ropivacaine sub-facially from the umbilicus up in the center part of the abdomen where we’ve closed the muscle up to the xiphoid. The whole abdomen becomes numb and the patients are gone within about 45 minutes to an hour after a tummy tuck or breast surgery. It has been fantastic.
8. What you see is what you’ll get, reducing risk.
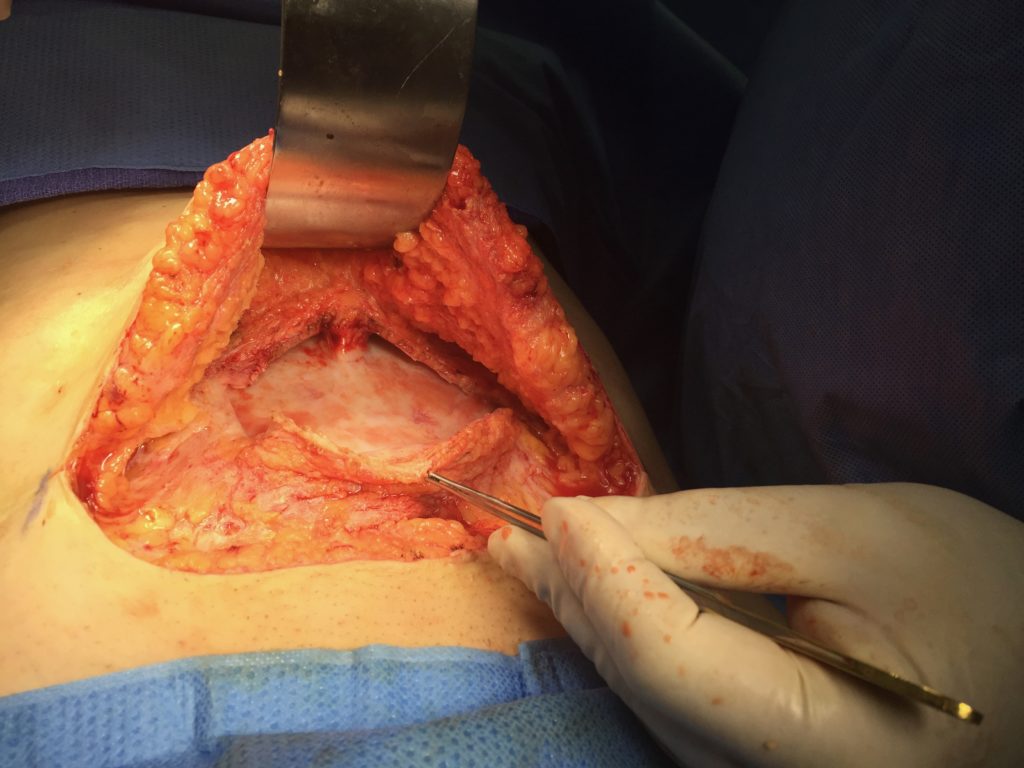
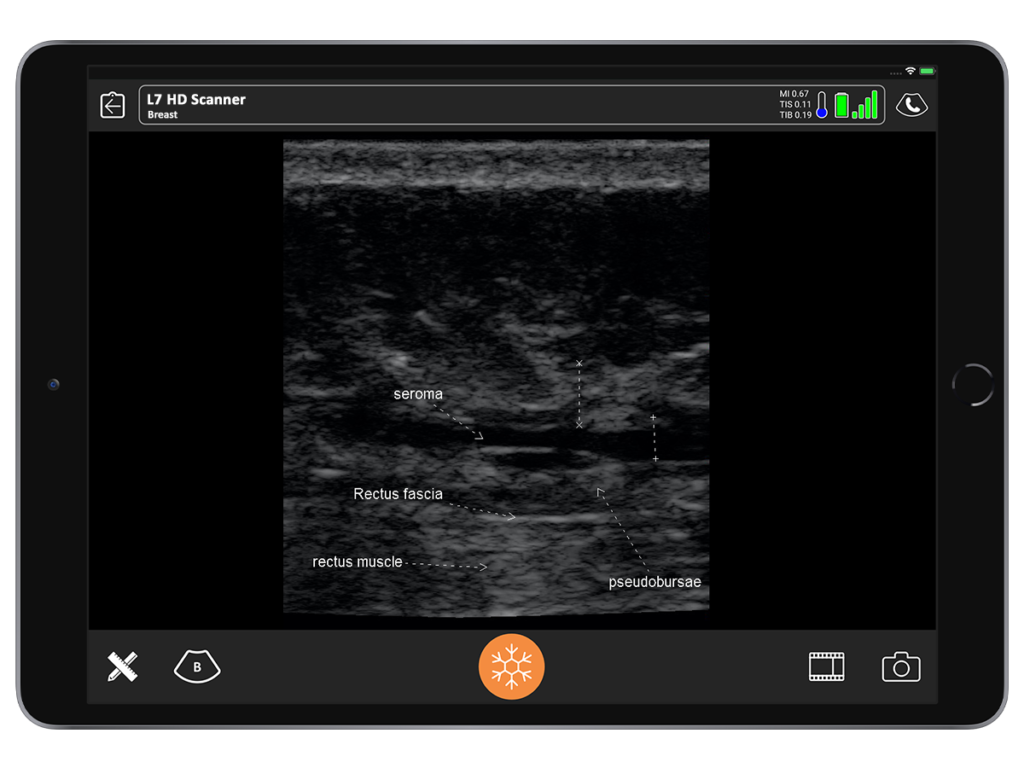
One of the coolest experiences I’ve ever had with ultrasound was being able to clearly see the clinical correlation between what I expected to see and what was actually there. I inherited a patient who had an abdominoplasty 12 to 14 months prior by another surgeon. She had developed a chronic seroma that had been aspirated half a dozen times. A sclerosing agent had been put in to try and stop the fluid buildup. She had both in and out indwelling drains.
When I examined the patient, I noted a huge contour deformity. I knew the plastic surgeon who performed the procedure would not have left this degree of irregularity with liposuction or with the underlying muscle.
When I placed the ultrasound device on the deformity, I could see a black hole that extended all the way up to the area of undermining, from the pubis, around the umbilicus all the way up to the xiphoid. Around that anechoic fluid was thick sclerotic fat. Although I had never seen this, I diagnosed it as a pseudo bursa. I predicted it would look like an orange peel with grungy-looking material on the inside and fluid.
When we saw it in the operating room, it looked exactly as I had seen in the ultrasound. It was the same size. I found it very satisfying.
9. Choose a handheld ultrasound that’s easy and affordable.
Ultrasound used to be intimidating to learn and expensive to buy. Users had to learn to adjust complicated knobs and buttons in addition to recognizing anatomy. Today’s handheld ultrasound scanners, which work with your phones and tablets, are intuitive and easy to learn, especially for plastic surgeons. We know what lies beneath the skin and where it is supposed to be. Hand-eye coordination is important in everything we do and we’re used to thinking about the body in three dimensions.
I’ve used many types of ultrasound machines over the years. For the last two years, I’ve been using a Clarius HD handheld ultrasound system. I love the fact that it’s wireless and has a much better image than my laptop system, which had cost me five times more.
I use it with an iPad, which everybody my age knows how to use. The Clarius software is intuitive and you just tap, pinch and swipe the touch screen to run the system. I have set up the buttons on the Clarius scanner to freeze and save images so I don’t have to touch the screen during the procedures. It’s easy to maintain a sterile field during procedures.
Instead of annotating images during the procedure, we store our images on the Clarius Cloud, which is included with the cost of the system. When I have time, I can then annotate and download the images directly into the patient’s chart.
10. It’s always fun to use ultrasound.
If you have a practice that’s anything like mine, you’ll use ultrasound every day. I look at patients all the time because I’m always learning.
I encourage new users to start with a training course to learn the basics and go through a series of simulations. I used to run hands-on workshops, but now with COVID-19, we’re running online courses, including with the ASPS. I have also recorded training videos with Clarius.
Once you have training and you’ve purchased a system, I recommend you start by examining every patient. Look at every single breast. Look at it even in week one when the patient comes back. See what the fluid looks like around the implant. Look at every single tummy tuck you do. You’re going to see seromas in every single tummy tuck. And then, if you want to start aspirating, you can start with an abdominoplasty. It’s pretty simple. Follow that needle and aspirate seromas.
I have yet to see a plastic surgeon who couldn’t learn ultrasound. Just buy it and do it. You will be good at it in a couple of months!
To learn more about how easy and affordable it is to add Clarius HD to your plastic or cosmetic surgery practice, contact us today or request an ultrasound demo. Together, we can explore additional advantages of choosing a wireless high definition scanner.