By Greg Fritz, PT, DPT, RMSK
The fields of orthopedic surgery and physical therapy are extremely vast and constantly changing. Every year, new diagnostic and therapeutic approaches are adopted and discussed in clinical studies and scientific papers.
However, ultrasound remains one of the most effective ways to diagnose and evaluate the different musculoskeletal structures during a lesion.
This fantastic machine allows physicians to accurately diagnose the underlying condition that’s causing the patient’s symptoms in a matter of minutes. It is non-invasive, safe, effective, and affordable.
This webinar discusses the general approach to musculoskeletal injuries and how using ultrasound can facilitate this process.
How to make a differential diagnosis.
Creating a list of diagnoses is an essential part of medical management as it allows physicians to narrow down the potential diseases that are causing the chief complaint.
To mediate this, there are some well-documented steps that all physicians need to follow when examining a patient with musculoskeletal injury.
Step 1. Get a history of the patient
Taking a thorough history of the patient is absolutely crucial to move forward in the management plan. By asking the patient the right questions, doctors can comprehend a great deal about the chief complaint, associated symptoms and any other medical conditions.
The answers will orient the physician towards a specific set of potential diagnoses, using one of the following methods.
Pattern recognition
As the name implies, pattern recognition relies on the physician’s exposure to diagnoses and chief complaints that allows him/her to come up with the best possible diagnosis that explains the patient’s signs and symptoms.
Scientific hypothesis
This step involves asking a question about the probability of a certain diagnosis.
Once a medical condition is suspected, the physician will try to assemble the information from the patient’s history and the findings of the physical examination to decide whether the diagnosis is reliable.
Step 2. Use critical reasoning and testing
When the doctor has a list of differential diagnoses, it is time to refine that list. By using critical thinking and findings of the physical examination, the list of diseases will get narrowed, which allows for the prompt posing of the diagnosis.
In physical therapy, the testing relies on examining muscle strength, joint range of motion and ligament integrity.
Step 3. Come up with a working diagnosis
All the steps above aim to answer one single question:
What is the working diagnosis of this patient?
In order to answer that, the doctor must collect the necessary data from all the phases of the diagnostic approach. In most cases of musculoskeletal complaints, it is difficult to confirm a diagnosis without imaging and blood tests. For this reason, ordering an imaging test might be a great idea to narrow down the list of differential diagnoses.
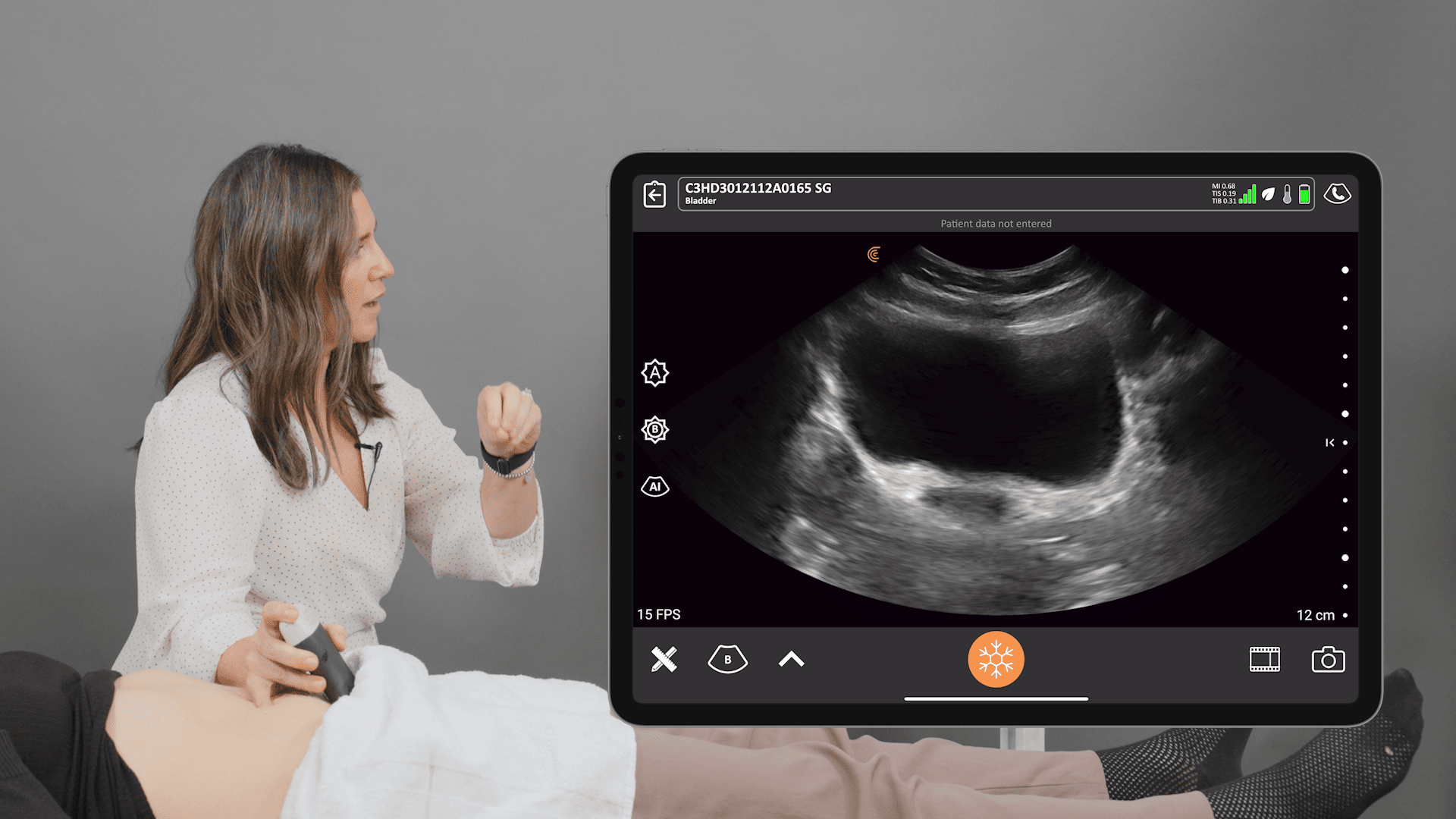
By far, ultrasound is the most commonly ordered imaging test in the field of physical therapy due to the benefits cited above (e.g., availability, affordability, accuracy).
The next sections detail how ultrasound can help us diagnose musculoskeletal injuries with high precision.
Helpful questions for differential diagnoses when using ultrasound.
Performing an ultrasound to narrow down differential diagnoses requires being systematic and organized, as well as asking the right questions.
Here are some primordial questions to ask when examining the patient with ultrasound:
- Are the ligaments or tendons involved?
- Is the integrity of the bones preserved?
- What’s the inflammatory status of the lesion?
- Is arthritis involved?
- What’s the origin of the symptomatology?
- How is the patient using his/her muscles?
- What’s the nature of the lesion under ultrasound?
- Is the lesion healing?
Reviewing all the possible answers to these questions is beyond the scope of this webinar. However, let’s review the importance of the first question when using ultrasound.
The role of ultrasound in identifying ligamentous lesions.
Ligaments and tendons are important structures that stabilize the entire musculoskeletal system. Unfortunately, they are also susceptible to a variety of traumatic and inflammatory conditions that disrupt their integrity and cause a wide range of signs and symptoms.
When using the ultrasound, you can check for any compromise that affected these structures and the degree of disruption, if present.
For instance, if one patient presents with signs and symptoms that suggest an issue with the ligaments or tendons, the ultrasound can tell us whether the cause is a sprain/strain or a tear.
Additionally, we can assess the degree of that tear to determine whether it’s partial or complete.
Case study
A 45-year old female who was on a skiing vacation in a Canadian resort presented with lateral knee pain. When asked about the origin of her injury, she stated, “I was queuing for the lift when I caught a tip under skis ahead, resulting in an unbalanced fall associated with a snap feeling in my knee.”
The patient felt immediate pain that was exacerbated with weight-bearing and a concerning instability when standing on one foot and trying to turn. She also stated that her pain was maximized when extending her knee, with minimal swelling during the acute phase.
When arriving at the emergency department, an X-ray was ordered, which showed no signs of injury. The woman left with an extension brace and an oral prescription of NSAIDs.
Four weeks after the accident, the patient was referred to my clinic to further assess her injury. Upon physical examination, the patient had no swelling or discoloration, but tenderness was present when palpating the fibular head and the lateral collateral ligament.
During the manual testing, Varus testing showed lax endfeel and triggered a sensation of nausea. The stability of the knee was preserved and meniscal testing didn’t show any conclusive findings.
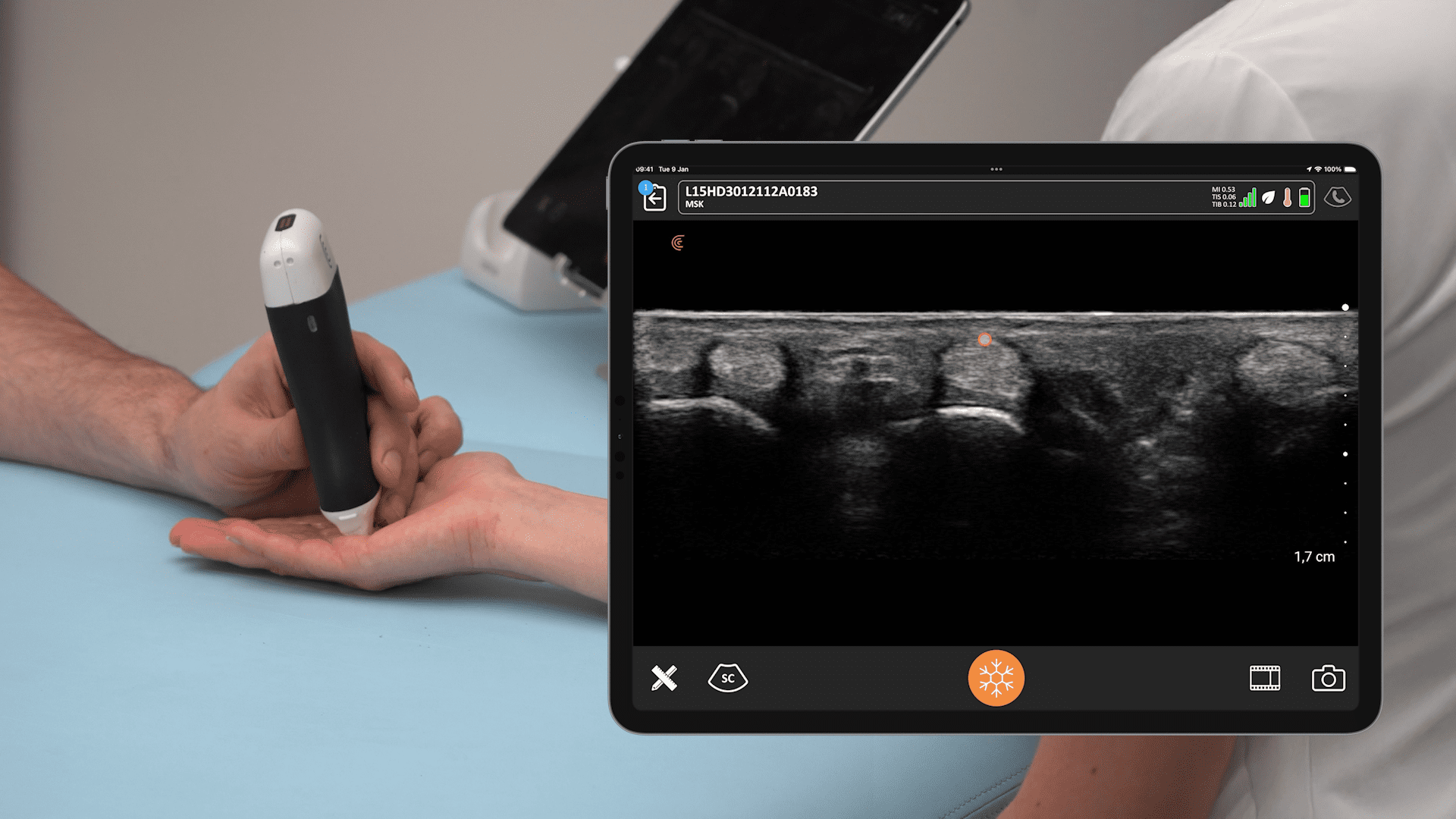
Ultrasound settings
To understand the findings observed on ultrasound, we need to appreciate the anatomy of the knee capsule. In the figure below, you can see that the joint capsule extends above the femur and under the quadriceps, which is referred to as the suprapatellar pouch.
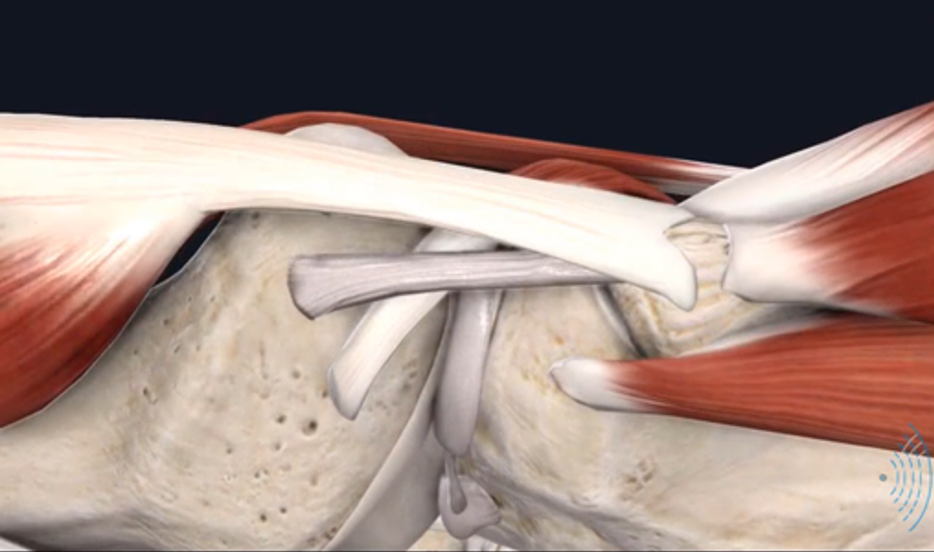
This area is predilected to intraarticular effusion, where fluid accumulates inside the joint capsule, causing the entire articulation to puff up. More specifically, the suprapatellar pouch can easily get effused with fluid, which is an important sign that can guide us towards one of the following pathologies:
- Cruciate ligament tears
- Meniscal lesions
- Osteochondral lesions
- Aggravated DJD
- Inflammatory arthropathies
- Synovitis
- Post-operative bleeding
The images below showcase the ultrasound findings of the patient in our case study:
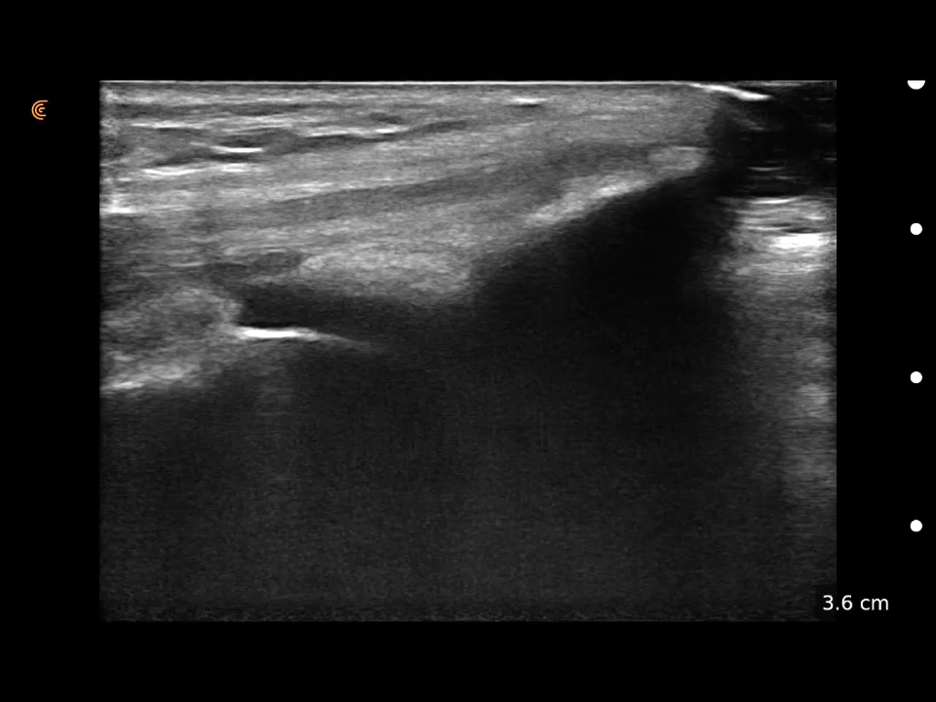
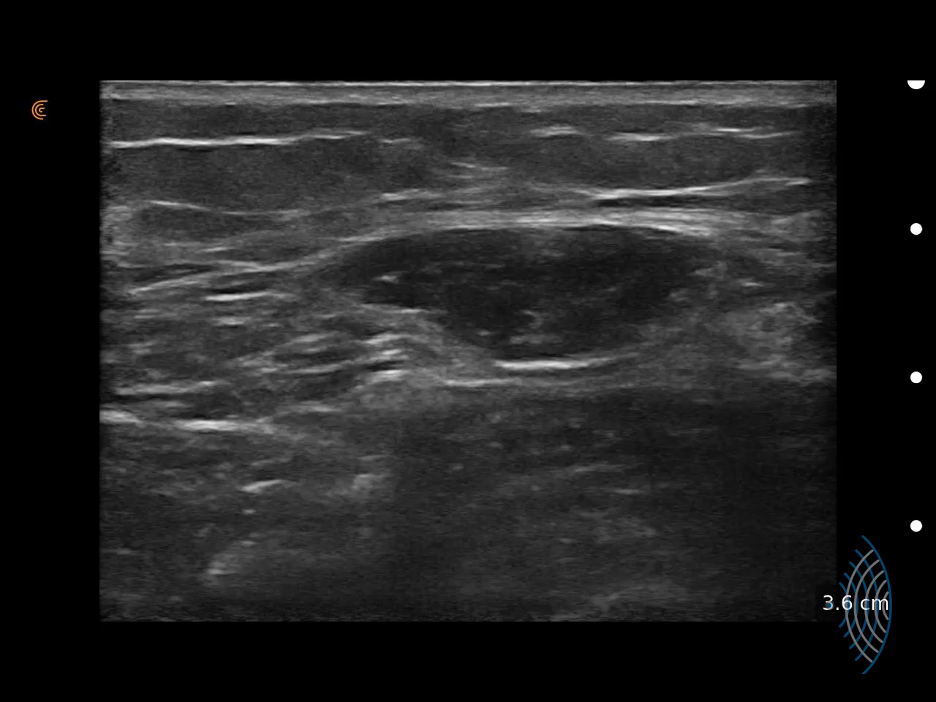
Interestingly, these images show no intraarticular effusion in our patient, which eliminates several potential diagnoses (e.g., ACL, meniscal injury and osteochondral lesions).
For reference, you can compare figures 02 and 03 to figure 04, which represents the pathological fluid accumulation in a patient with knee trauma.
For those of you with good eyes, you might notice a small buildup of fluid in the first and second ultrasound images, which is just a physiological accumulation of fluid that exists to facilitate the friction between different components of the articulation.
Once the internal aspect of the knee joint was thoroughly investigated and showed no signs of effusion or trauma, it was time for the inspection of the lateral aspect of the articulation, which contains several complex structures that are prone to injury.
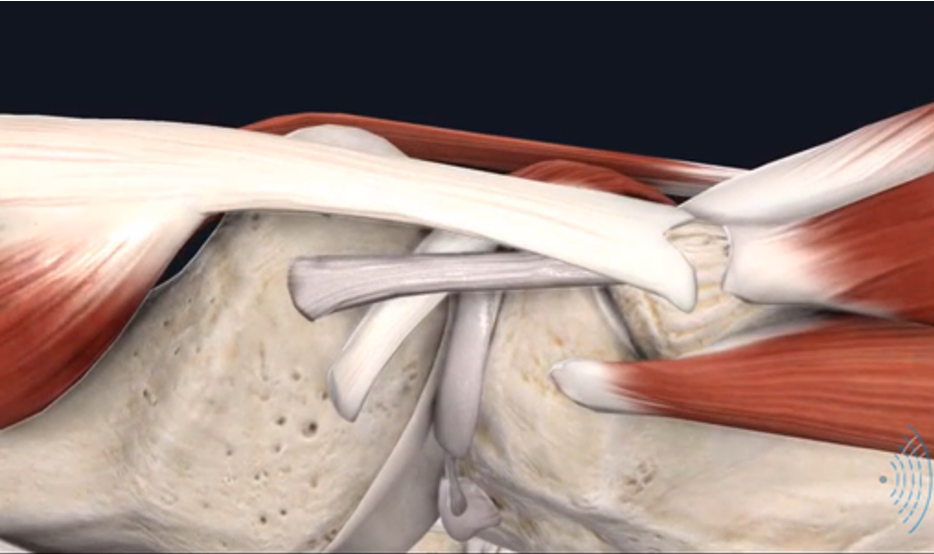
Figure 05 demonstrated the anatomy of the lateral aspect of the knee, which also corresponds to where our patient pointed to her pain.
This side contains the following structures:
- The lateral meniscus
- The popliteal tendon
- The biceps femoris
- The lateral collateral ligament
When I used ultrasound on the lateral aspect of the knee, the following image was generated:
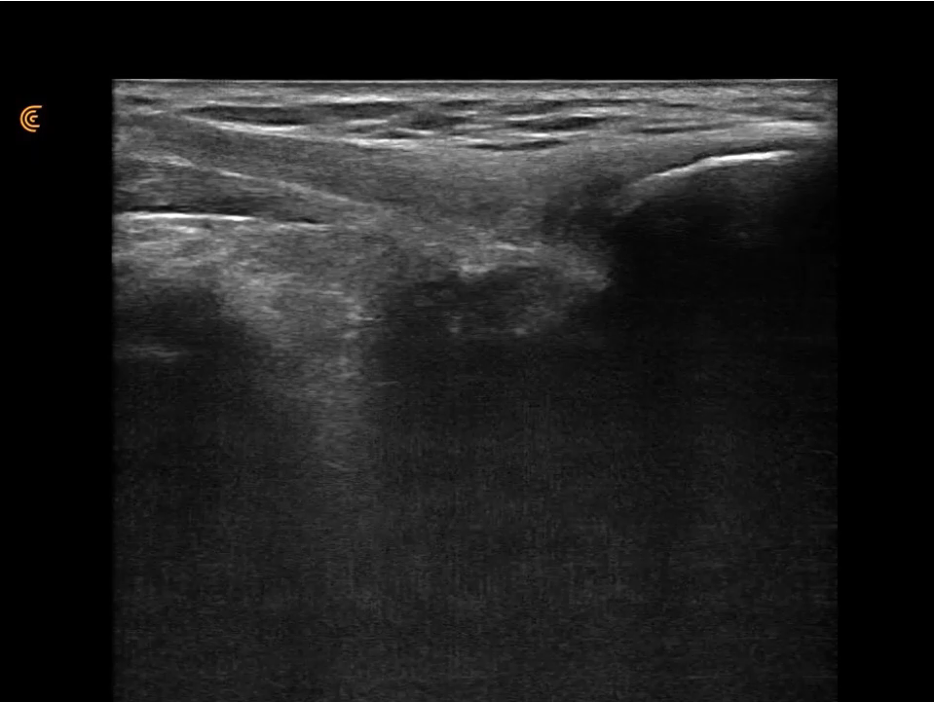
While this figure shows some darkness between the biceps femoris tendon and femoral head, it is not that significant to confirm the diagnosis of tendon tear.
To have a better visualization of the lateral side of the knee, I decided to sweep the probe above the lateral collateral ligament (LCL).
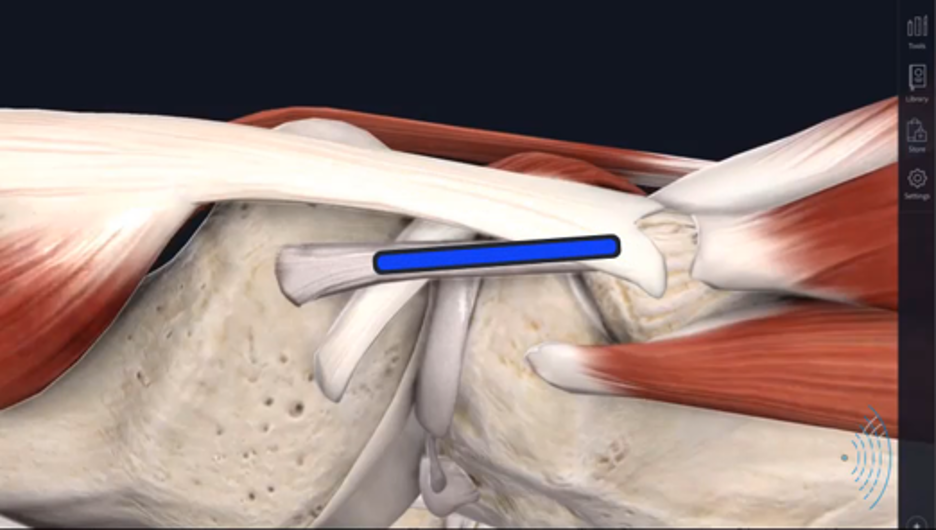
The following video demonstrates fiber compromise that separates the lateral collateral ligament and the fibular head, which is a finding worth further investigation to precisely locate the site of injury.
By placing the probe of the ultrasound on the lateral collateral ligament, I captured the following video:
As you can see, the fibers of LCL attach to the lateral condyle and then extend to reach the fibular head. However, the interesting finding in this video is the fluid accumulation found distally and above the LCL.
This effusion clearly demonstrates tears of the LCL fibers.
This region of the fibular head has some unique imaging characteristics that can seemingly demonstrate interfibrillar effusion or fluid, when in fact it may be a characteristic of the insertional fiber orientation (anisotropy) of the biceps femoris attachment to the fibular head. One should always consider the clinical presentation and interrogate color doppler before they conclude it is an active, effusive, inflammatory response.
Aside from fluid detection, the ultrasound scanner is also equipped with a tool (doppler) that allows us to visualize excess blood flow.
Since ligaments and tendons are avascular structures (no microscopic blood vessels inside them), any signs of neovascularization in the LCL will be considered a pathognomonic sign of inflammation.
This time, however, I ran the probe as shown in figure 08.
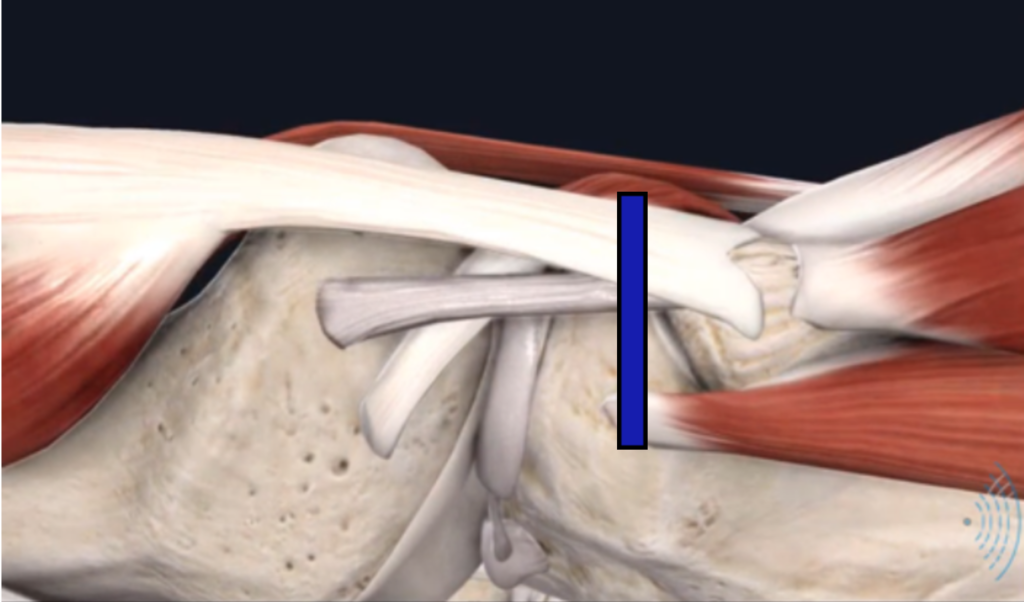
During the ultrasound, I found excess blood flow between the biceps femoris tendon and the LCL (insert the video below), which is a clear sign of inflammation.
To summarize, the findings above allow us to conclude that there is an inflammatory reaction that’s triggered by a lesion in the distal portion of the lateral collateral ligament.
Takeaway message
Ultrasound is a useful diagnostic tool that allows for non-invasive, accurate and affordable assessment of the musculoskeletal system.
The use of ultrasound for the patient in the case study allowed us to answer the following queries:
- The chronological aspect of the lesion – healing phase
- The compromised structure as well as the affected portion – the distal portion of the LCL
- The degree of the lesion – inconclusive
- The need for MRI and/or a surgical consultation – positive
- The involvement of osseous structures – no signs
- The phase of healing – inflammatory phase
Hopefully, you found this webinar informative. To learn more about which Clarius HD scanner is right for your MSK practice, visit our page on Handheld Ultrasound for MSK.