Clarius Webinars featuring Dr. MJ Warmann Rowland are always popular and highly rated. That was particularly the case with this one: Ultrasound-Guided Techniques to Rapidly Dissolve Fillers, Part 1: Misplaced Facial Fillers. The one-hour episode is available now to watch at your convenience. Scroll below for a few highlights.
Dr. MJ shifted from general dentistry to complete her master’s in orthodontics and aesthetic medicine. Today, she practices non-surgical aesthetics with a special interest in managing dermal filler complications using ultrasound. Overcorrection or misplaced filler is one of the most common complications she sees in her practice. Besides being aesthetically disappointing, this can cause physical or psychological issues for patients.
Why Use Ultrasound for Aesthetic Medicine
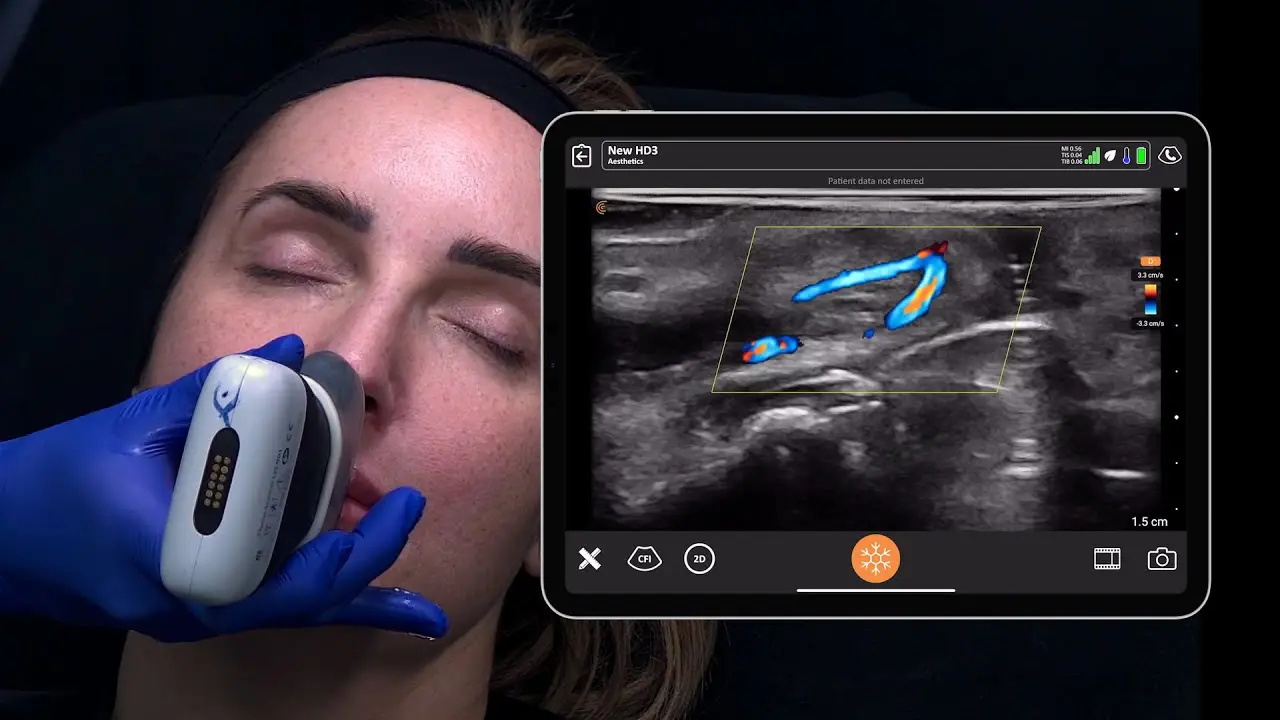
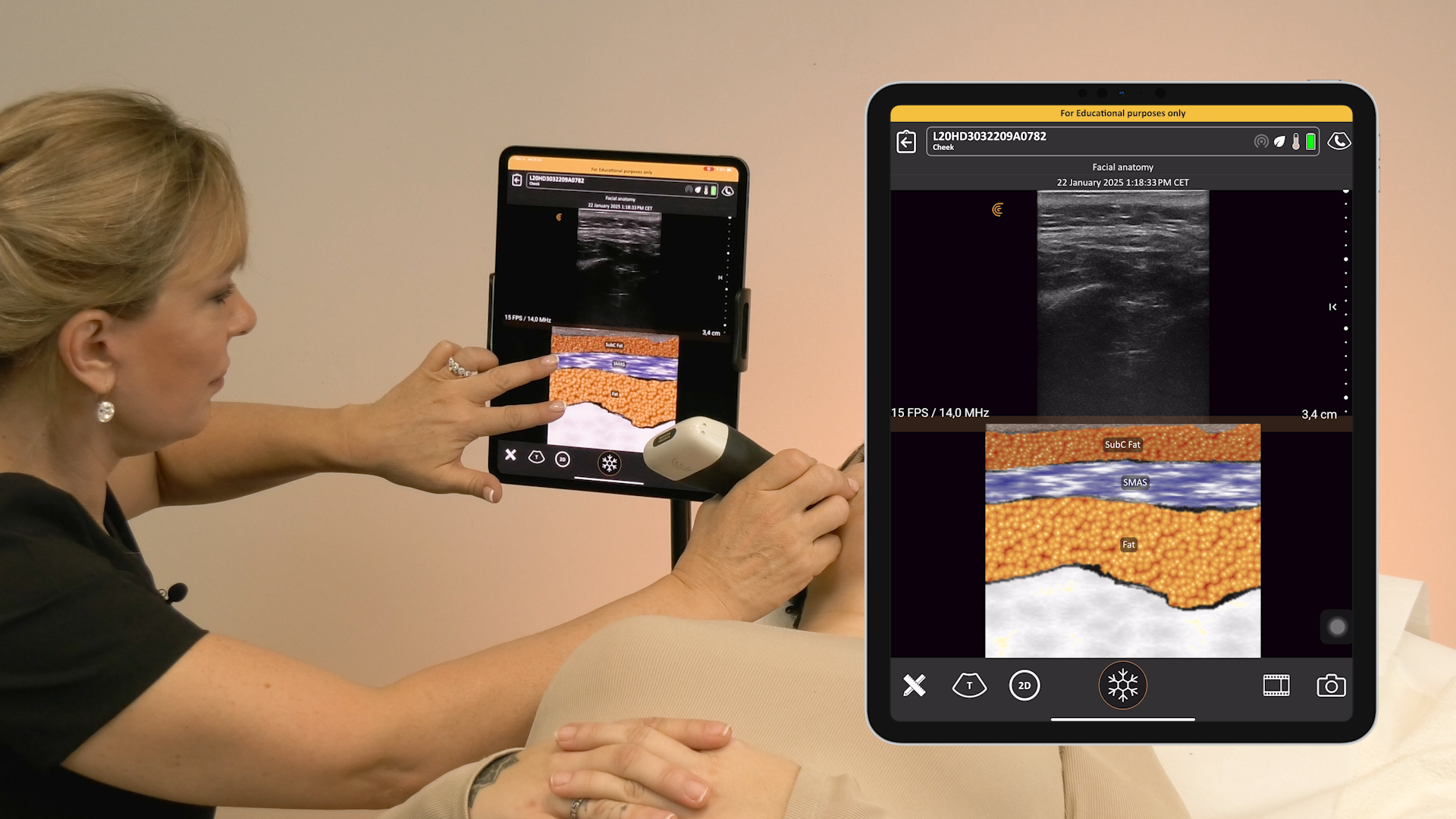
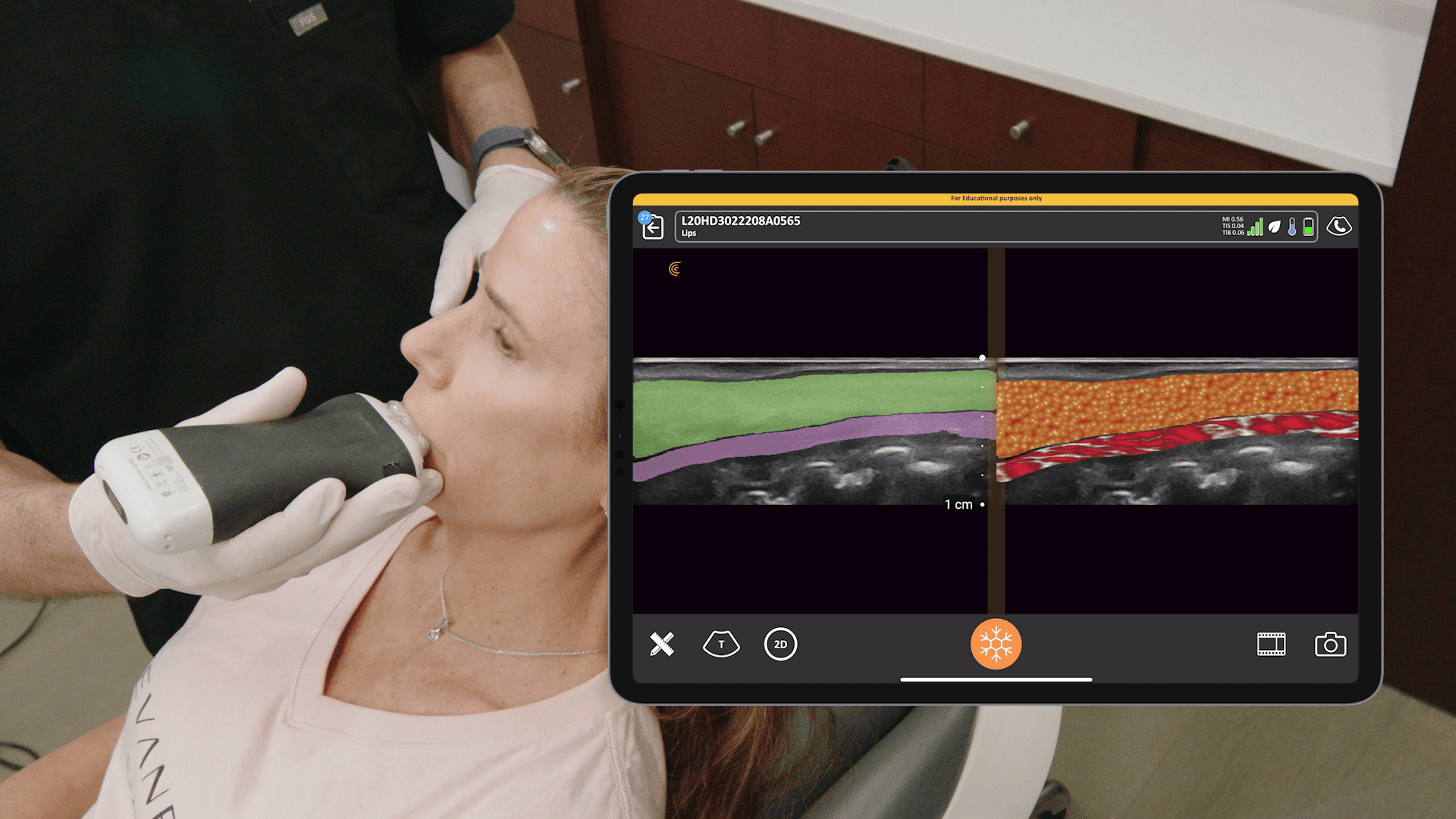
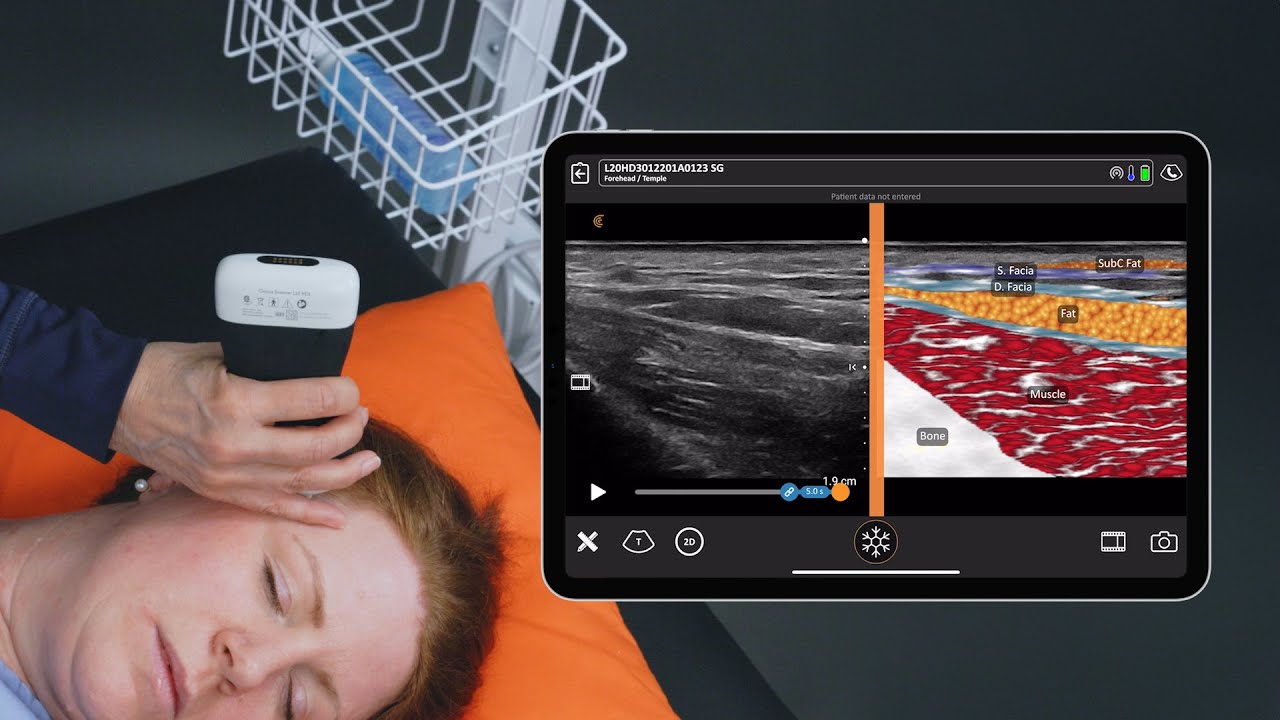
Dr. MJ has been using the Clarius L20 handheld ultrasound for her practice for two years and says using it for filler treatment “is a godsend, whether that be before treatment to vascular map, during treatment to place filler using ultrasound guidance, or after treatment to confirm placement.
It is key to predictable outcomes. We can check up on our filler over time, and decide what’s hidden in our patients‘ faces if we come across historic filler, and we can learn a huge amount of anatomy using it in our daily practice, but one major use is in dermal filler complications. Diagnosing and managing complications has arguably taken a giant leap forward since ultrasound. Being able to see beneath the surface of the skin to identify problems from filler is revolutionary. Gone are the days when we’re left guessing what the problem is or even where the problem is. Now, this simple two-minute diagnostic can help us resolve problems swiftly and effectively.”
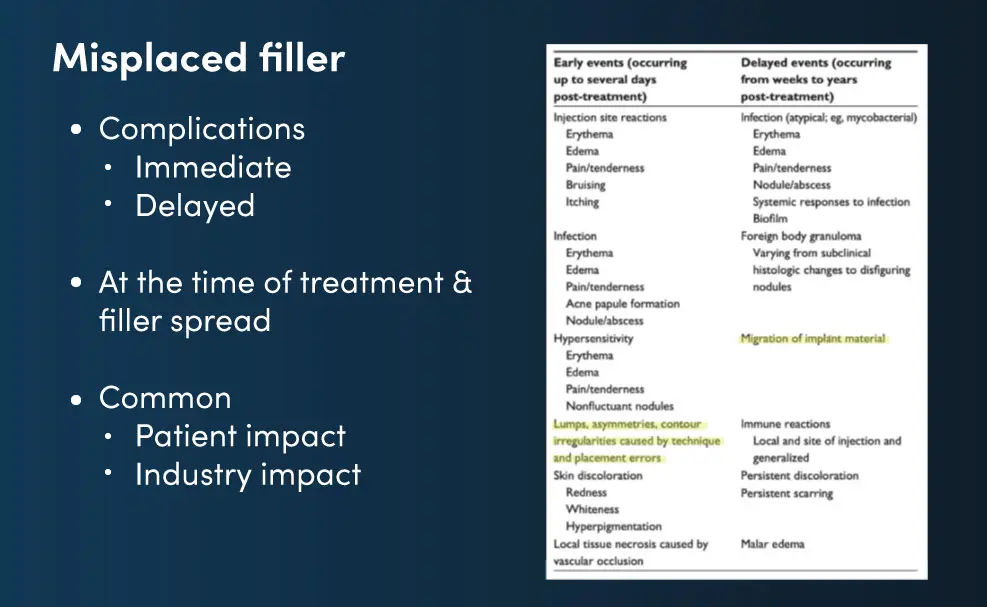
Overview of Adverse Reactions of Misplaced Fillers
CASE: Tear Trough Filler Causing Bilateral Interorbital Swellings
This patient presented with bilateral interorbital swellings, which have been there since she had tear trough filler 18 months ago. They’re not painful. They don’t fluctuate, but they’re unaesthetic. She was told by her injector that the filler had gone after all this time. But as we know from recent studies, like the 2021 by Mobin Master, filler sticks around for years if not decades. So, this is a classic case of an immediate complication not being handled and turning up delayed.
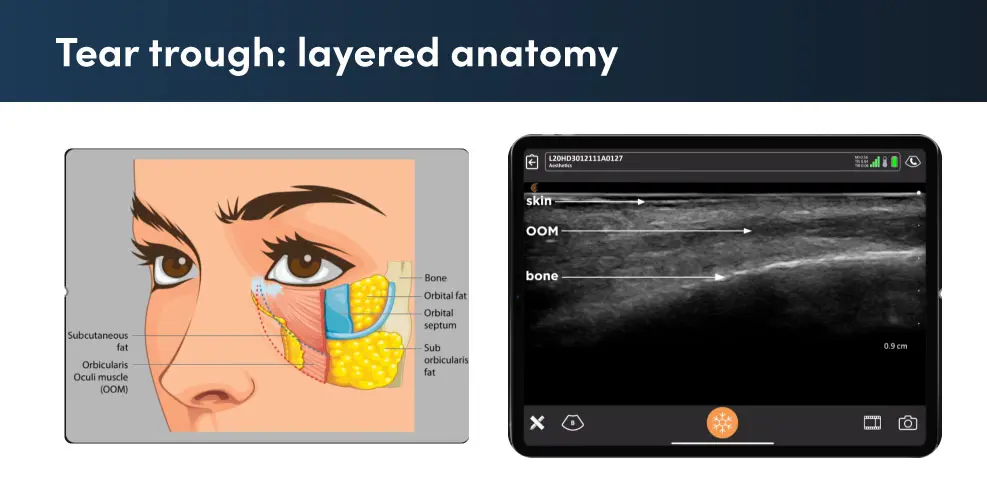
Dr. MJ provides a detailed review of the case and tear trough anatomy during the webinar. Watch this video to see her technique for dissolving tear trough filler. Instead of using a “shotgun approach” that floods the area with 1500 units of hyaluronidase, she pinpoints the area with ultrasound and uses a much lower dose with better results.
Q&A: Which needles are you using when injecting hyaluronidase?
Dr. MJ Rowland-Warmann: I don’t use a cannula. I use a needle. I use a 27-gauge, one- and three-quarter-inch standard needle, not anything highly reflective. You can see that perfectly well on the Clarius. I would say the imaging that I get is great. The problem that you’ll have is lining it up. You’ve got to make sure that the needle is directly in line with your transducer, and that it doesn’t deviate. That’s where all of the problems come from. So, you’ve got to develop an eye for keeping that needle in line with the transducer, and you will get brilliant results even with a 27-gauge needle like I use.
Q&A: Are you using lidocaine for your injection entries?
Dr. MJ Rowland-Warmann: Yes, I sometimes do. I often dilute the hyaluronidase itself with four parts saline, and one part lidocaine so that it’s less painful for the patient. I found that works quite well. I use in total a five-milliliter dilution of 1,500 units of hyaluronidase.
Q&A: Would you say all misplaced filler remnants can be dissolved? In essence, can a patient gain back absolute original features?
Dr. MJ Rowland-Warmann: Are we going to put them back to a time ago before they had filler? The answer is no and never. There are multiple factors that contribute to a complication, and the filler itself is just one of them. If we remove the filler, the filler might be gone, but the complication itself has effects on the tissue, so there may be an adaptive response, and some of this adaptive response is hypervascularity that you see. Some of it may be edema of the tissues. Sometimes around the tear trough, that doesn’t completely go.
We also have two other factors. One of them is time. People age. If you’ve had a longstanding complication, me removing that filler is not going to put you back to where you once were. That has to be very carefully managed, and patients need to be instructed on that.
The last is perception drift. People always seem to remember themselves as better than they were. Objects in your memories are always seen with rose-tinted spectacles. So, the phenomenon of perception drift is patients always perceive themselves as complete before the complication.
When you remove that hyaluronic acid, and you leave them with the effects of time and potentially with the effects even minor of the complication, sometimes they’ve become quite despondent. So, management is very crucial at the start that that is done properly, but the actual hyaluronic acid filler itself, yes, can be removed in most cases. There are some rogue fillers out there on the market, especially in Europe where we are a little bit less licensed, that are much more difficult to remove. Obviously, permanent fillers cannot be removed with hyaluronidase.
Watch the webinar to learn more from Dr. MJ. You’ll also receive a 20% coupon for online courses at the Smileworks Training HUB.
Affordable, High-Definition Ultrasound for Aesthetics
Wireless and pocket-sized, Clarius handheld ultrasound scanners deliver the high-definition imaging and performance of traditional ultrasound systems for a small fraction of the cost. They are the leading choice for plastic surgeons and aesthetics practitioners performing ultrasound-guided procedures to ensure patient safety.
New T-Mode™AI by Clarius is a groundbreaking educational technology to help clinicians new to ultrasound advance their image interpretation skills using Clarius handheld scanners.
Visit our aesthetics page to learn more or request a virtual ultrasound demo today to learn how high-definition ultrasound imaging with voice controls can improve safety and deliver consistent patient outcomes at your aesthetic practice!