In a recent webinar on ultrasound-guided pain procedures, renowned pain management expert Dr. David Rosenblum shared practical remedies for treating chronic pain. Focusing on a specific case, Dr. Rosenblum provided step-by-step instructions on how he performs an occipital nerve block using ultrasound guidance.
Watch his Clarius Classroom video demonstration of an occipital nerve block and read on for more detailed tips from Dr. Rosenblum.
Treating a 60-year-old Female Presenting with Severe Chronic Neck Pain and Headaches
«This patient has a history of rheumatoid arthritis and lumbar spine fusion. She presents with occipital pain radiating upward and forward bilaterally. Occasionally, the pain is retro-orbital. It’s a dull pressure like pain rated nine out of 10 and is worse with stress.

With the occipital headache, we see pain radiating in the occiput. This is secondary to either compression of the nerve, fibrosis or the muscle spasm. It’s very similar to the cervical genetic headache, which originates in the cervical spine. The C2 and C3 nerve roots do contribute to the occipital nerve, so there’s definitely a connection. In these patients, you may see pain radiating anteriorly, especially retro-orbitally. There is connection between the occipital nerve and the trigeminal nerve at the top of the head, which explains this phenomenon.
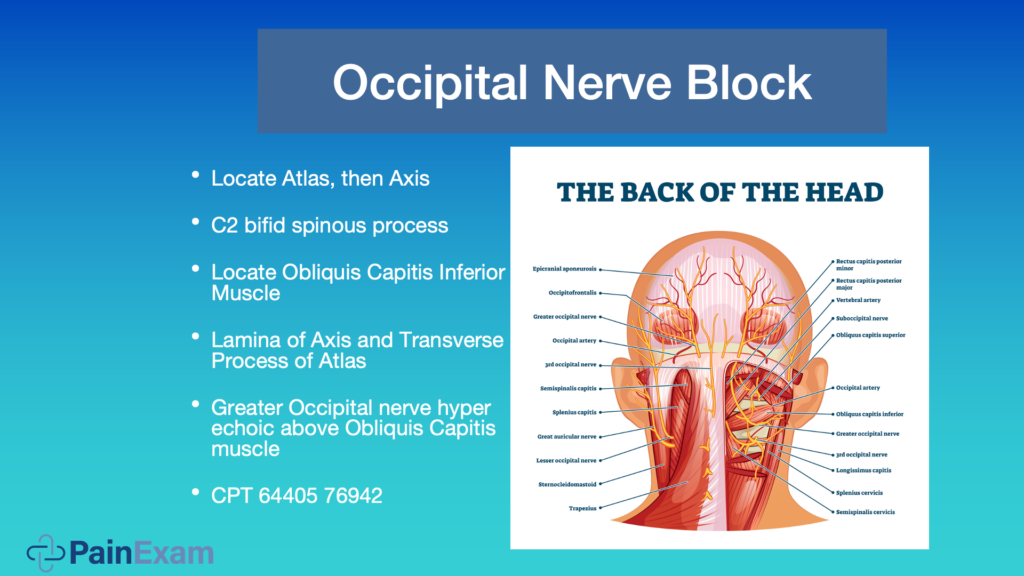
In the image above, we’re looking at the back of the head. If you’re doing this procedure using the blind approach, you may palpate for the pulse with your finger at the occipital notch, where you’re going to aspirate and inject. You give approximately four MLs of local.
With the ultrasound, I cut it down to one or two MLs of local and maybe steroid. The key is finding the level of C2 where the obliquus capitis inferior muscle is. The nerve forms after it exits the spine at C2 and C3 – go over that muscle, and ascend upwards. The muscle covering it is the splenius capitis muscle.
Above is an ultrasound view of the bifid C2 spinous process. You see the position of my ultrasound scanner. We scan the back of the head, axial cut and scan medial, laterally. In the ultrasound image, we see the occipital nerve is hyperlucent. Under it is the obliquus capitus inferior muscle overlying the C2 lamina, and then the splenis capitus muscle. I come in from a lateral towards medial approach when I perform the shot.
A Review of Cervical Anatomy
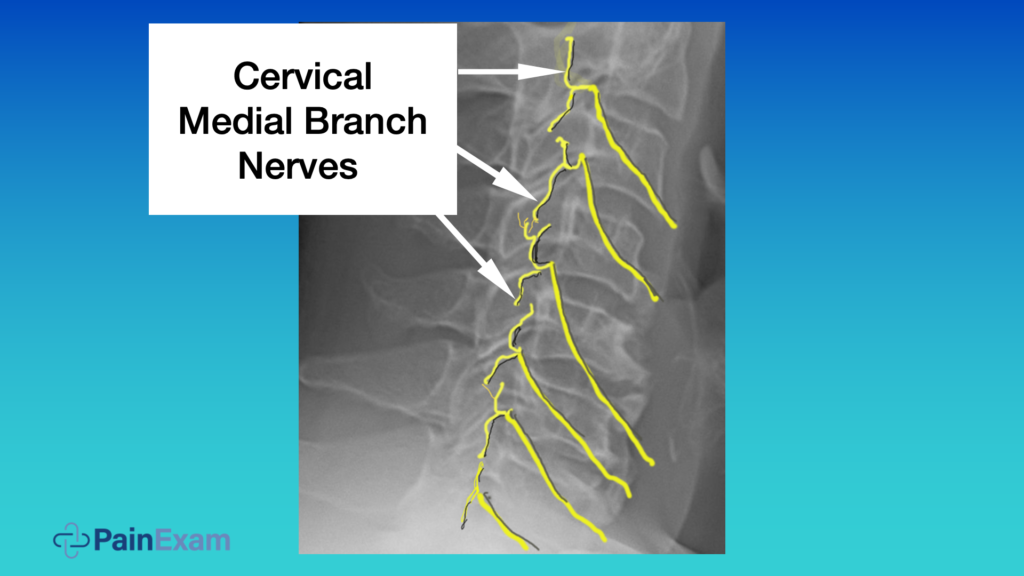
For this patient, I perform a block of the cervical medial branch as she had an occipital nerve block and some cervicogenic pain. Let’s quickly review the anatomy. The cervical medial branch nerves will innervate the facet joints in the neck as well as the paraspinal muscles. Each joint has two nerves innervating it and they run along the articular process. They come outside the frame and they run posteriorly, and they ascend and descend.
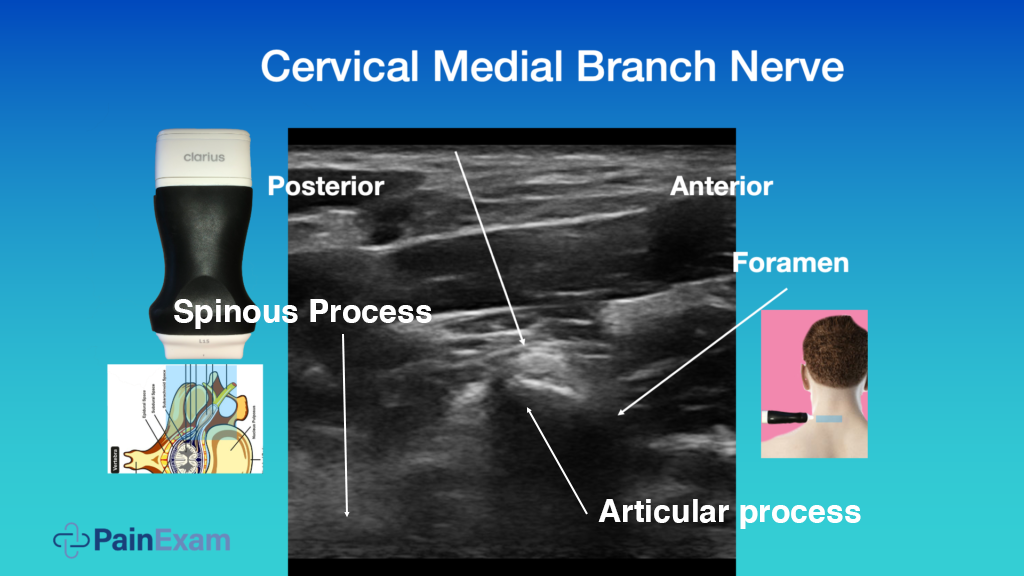
The ultrasound image above is from the side of the neck. It is almost an axial cut. This is the articular process. You see the foramen and the spinous process would be here. It’s the same orientation and you see the medial branch nerve is looping around backwards towards the facet and the paraspinal muscles.
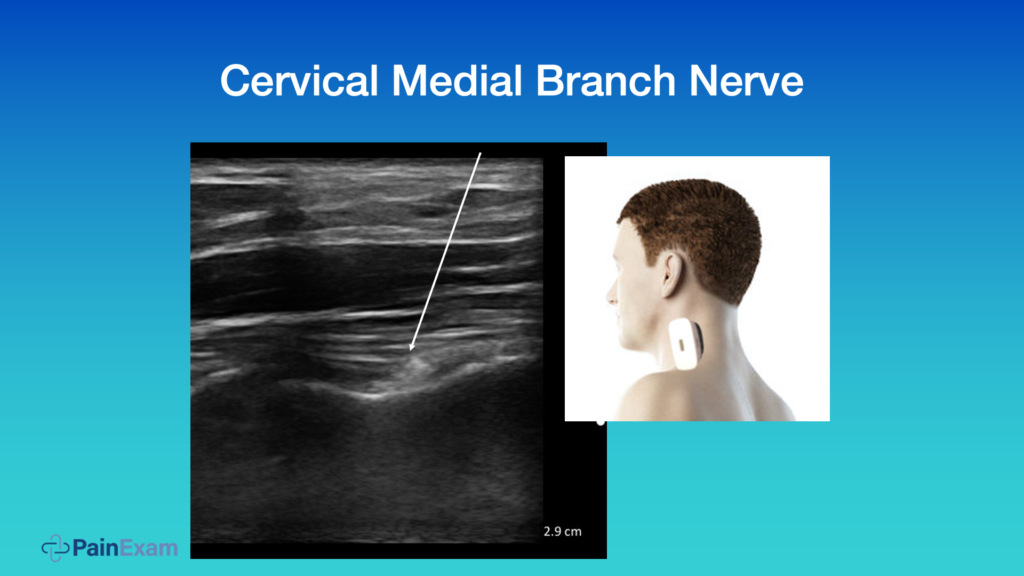
Above we see another view of that medial branch nerve in an oblique fashion. I don’t normally block the nerve in this way, but you can.
Video Demonstration: Occipital and Medial Branch Nerve Block for Symptomatic Relief
In the following video, I perform nerve blocks under ultrasound guidance to treat this patient who has cervical disc disease, facet arthropathy manifesting as cervicogenic headache, and occipital neuralgia. I perform an occipital nerve block and inject the medial branch nerves to alleviate the occipital neuralgia aspect of her pain, as well as some of the cervical genetic aspects.
I use a 25-gauge needle, which is thin, but you can still see it on the ultrasound image. With the out-of-plane approach, you don’t see the whole needle; just the tip. Be sure to aspirate and inject next to the nerve. You’ll see the medication spread over the cervical medial branches as blackness on ultrasound.
Because I used an ultrasound for the procedure, not a fluoroscope, I didn’t count the levels the same way. I actually counted downwards from the C2 transverse process. I anesthetized the C3 and the C4 medial branch nerve. The patient reported feeling better and I hope it will give her long term relief.
Note: I would never do a radiofrequency after this because I’m not labeling levels exactly. Nor would I ever recommend any surgical procedure based on my estimated levels. I’m just aiming to get some symptomatic relief, which you can see is very easy, quick, and cost-effective to do with ultrasound guidance.»
Watch the Webinar «Practical Pandemic Pain Remedy: Ultrasound-Guided Occipital, Erector Spinae & Tendon Sheath Injections»
Watch the full «Practical Pandemic Pain Remedy» webinar to learn more practical tips from Dr. Rosenblum. Or watch two more of his new Clarius Classroom video tutorials on how to use ultrasound guidance to safely perform an erector spinae block and a gluteal tendon injection.
Dr. Rosenblum is the Director of Pain Management at the Maimonides Medical Center in New York. A prolific educator, he hosts the Pain Exam Podcast and created a Pain Exam Board Review, which has helped more than 3,000 pain management physicians become board certified. Dr. Rosenblum’s program Private Ultrasound Instruction for Regional Anesthesia & Pain Management is available now on his Pain Exam website.
Dr. Rosenblum uses the Clarius L15 HD and L7 HD for his pain management practice. To learn more about how Clarius HD is used to guide injections, visit our wireless ultrasound for pain management page. Or contact us today to book a demo with one of our ultrasound experts.