Dr. Hirahara is board certified in orthopaedic surgery and orthopaedic sports medicine. In addition to running a busy practice in Sacramento, California, he speaks and teaches internationally with published research on arthroscopic shoulder and knee surgery, orthobiologics, and the use of ultrasound.
“We have to rethink how we do things and what we’re doing. The old way of trying to shotgun everything and get it to the region is dead,” says Dr. Hirahara.
“We now have sniper rifles and we need to be able to make good diagnoses and be able to specifically say what our goal is with this injection. We’re not just trying to diminish pain; we’re trying to promote healing.”
We recently had the privilege to host an educational webinar with Dr. Hirahara: Visualize Your Needle: Ultrasound for Painless and Accurate MSK Injections. Watch the webinar to hear what he had to say or read on for a few highlights from his one-hour presentation.
Dr. Hirahara’s Quick Tips for Using Ultrasound for Orthopedic Treatments
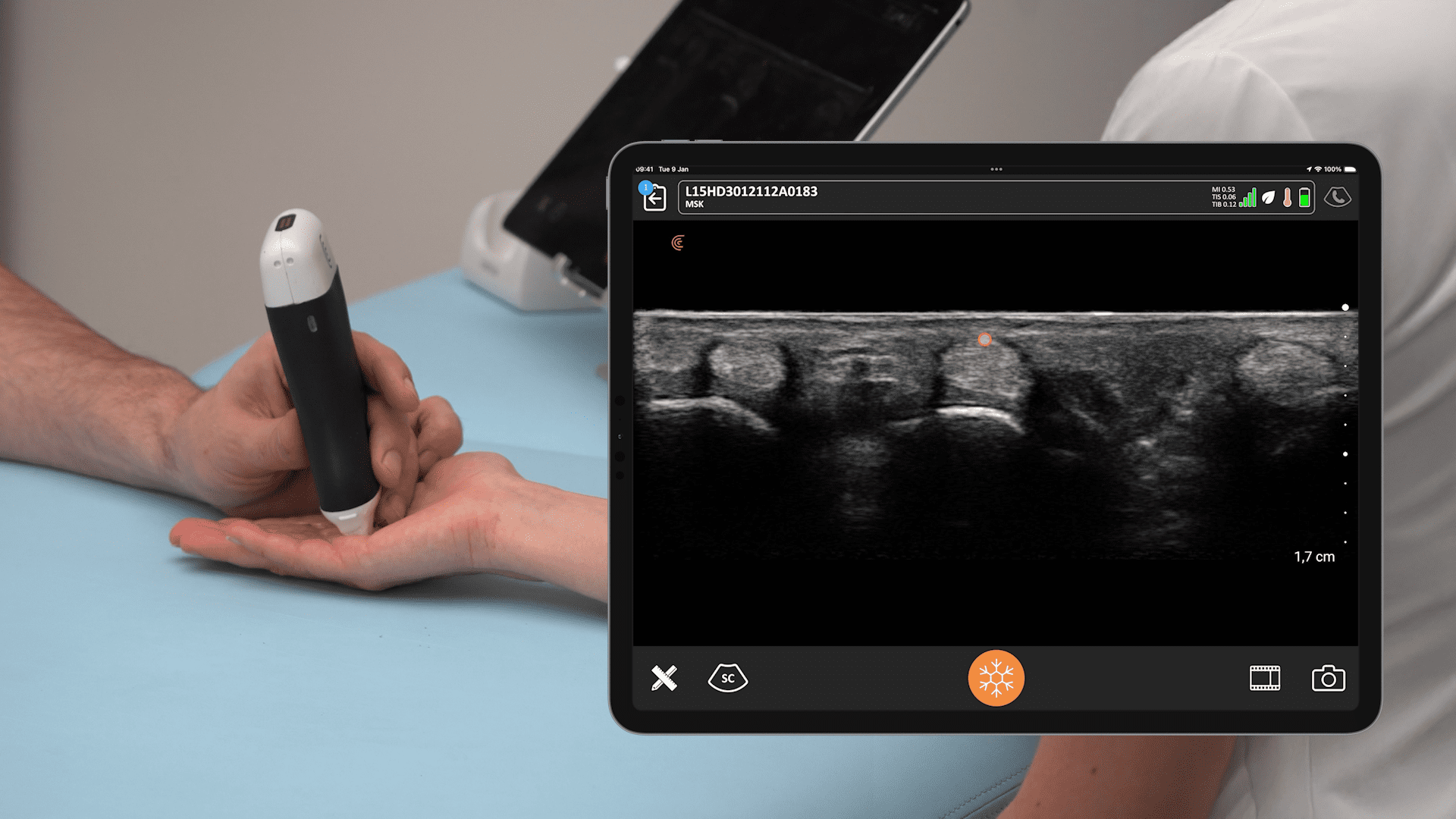
- Optimize your image – get a good image so you can make sure to see the tissue, the anatomy very well. It will actually improve your visualization of your needle.
- Stay perpendicular as possible to your tissues and your needle, it will make them pop.
- Look at the bone – the bone’s the key. If you’re perpendicular to the bone, it’s going to brighten up and that’ll help your entire image; everything else will look better.
- Pre-plan your approach, know how deep you have to go, know your plan, know your plan of attack, your angle. Do you want to angle down, at what angle, what steepness? Do you want to come in flat? What level are you going to start at; where’s your entry point?
- Use Doppler to check for vascular structures. I’ve seen too many people not even realize that there’s a vascular structure between you and where you want to go. Check to make sure you know.
- Choose the right needle length – Pre-determine if your needle length is going to be adequate so you can know how far you’re going to go. Plan it out because your needle length may be inadequate to get where you want to be.
Ultrasound-Guided Shoulder Injection
“I am a fellowship trained shoulder surgeon, and I used to think I was really good at blind injections. I figured I could hit that subacromial bursa easily. But as a surgeon, you also learn that the bursa is a potential space under the acromion. Even if you try to ride the acromion and come up, sometimes there’s muscle that sticks to that area and you’re not going to actually be able to get to that subacromial space as easily as you think you can.
The usual miss rate for shoulder injections without ultrasound guidance is very similar to knees; it’s around 30% for the subacromial bursa. And now we know that ultrasound guidance is critical even for the subacromial space.
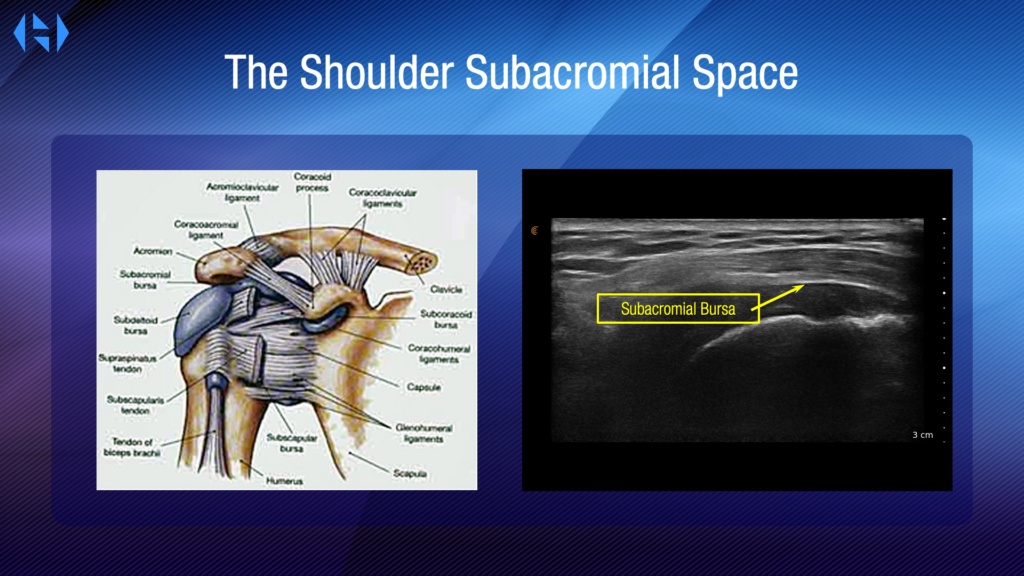
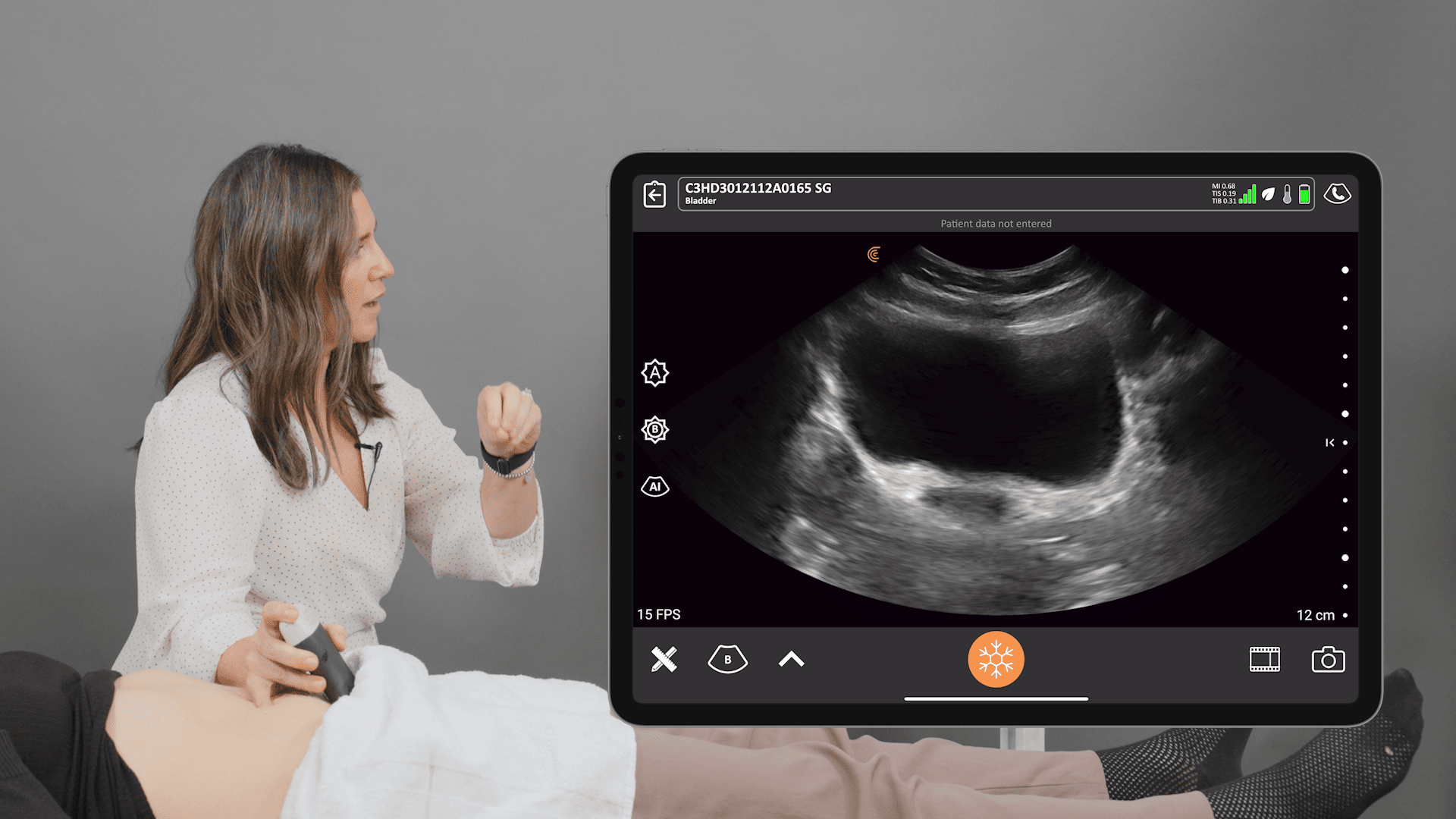
Taking a look at the anatomy. Just below the subacromial fat, you get the bursa. That dark area below that hyperechoic line is actually the bursa. So you’re looking for that hyperechoic line to go below; that’s where you want to be. The plane is important. So being able to image the shoulder properly is critical.
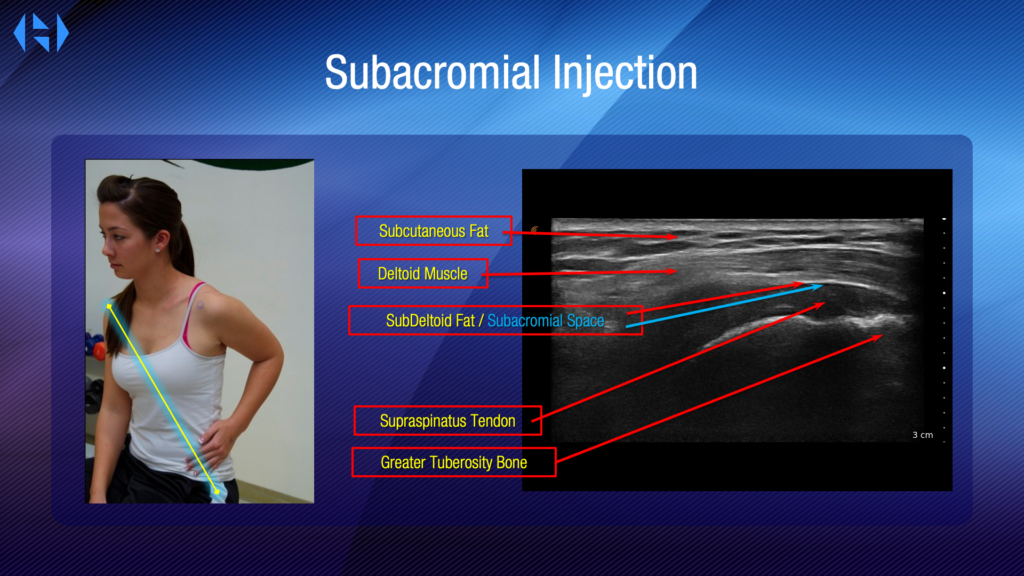
You could use the arm at the side, but it won’t show you as much of that supraspinatus tendon as you may want to see. Being able to bring that supraspinatus tendon out from under the acromion is critical. You simply take that ipsilateral hand; bring it to the ipsilateral hip, and tuck that elbow back making sure the arm is adducted not abducted. Now, taking the plane from the contralateral shoulder to the ipsilateral hip, that’ll be the plane that your probe will go on to be able to see. That’ll put you in line with your supraspinatus tendon, muscle, and tendon fibers.
This will give you that long axis of the supraspinatus. That’s what you want to look at. And here we can see it very clearly. You can see that humeral head outline, the roundedness. You can see that tuberosity. You can see the supraspinatus tendon and the bursal space. Starting from the top down, we see the subcutaneous fat, the deltoid muscle, the sub-deltoid fat, the subacromial space, the supraspinatus tendon, and finally, the tuberosity bone.
Now, when I say optimization, this video starts off non-optimized. You can see how I’m changing my angle to make everything more hyperechoic, denser versus less so. That’s what I mean about optimization. In this video, you’re going to see that I’m clearly not in a good plane; you don’t see things popping. But as I change my angle to be more perpendicular to the bone, the bone becomes very hyperechoic, you see that sub-deltoid fat becomes very hyperechoic. That’s the plane you want to be in. This is a way to optimize your image to see better so that when you bring your needle in the plane, you’re going to be nice and perpendicular, making the needle pop as well.
In the video below, you see a subacromial injection. You don’t see the hyperechoic line of the fat very well, but you can see me coming into image as things start to expand. I’m clearly in the right space. You can see how that hypoechoic fluid progressed medially immediately. So it wasn’t that I’d missed and wasn’t that I was in a fiber causing a small bubble; it was clearly in the space, filled the whole space up. »
Video: Performing a Subacromial Injection on a Patient with Surgical Adhesions
“Here’s an example of doing a subacromial injection on a patient who has surgical lesions. You’re not going to see that hyperechoic line and the sub deltoid fat because he had surgery in the past.
And you’re also not going to see the filling of the subacromial space as nicely because again, there’s going to be adhesions and so you have to keep that in mind. If someone’s had previous surgery, please be cautious that the anatomy is going to be distorted. It’s a little tougher to do, but you can still see where his subacromial space is and we can get into that pretty easily.
This procedure would be very hard to do completely blind. It would be hard because it wouldn’t have that nice filling effect in that release of the fluid as you’re pushing in. We’re really going to be almost hydro dissecting through the plane coming in and moving forward along that plane to make sure I actually open that space up between the supraspinatus and the deltoid. By looking at my image ahead of time, I’m able to see exactly where I want to come in. I see exactly my plan of angle and attack. I can go ahead and clean up a small area. I don’t have to clean up a large area. I use iodine, and I use an alcohol swab, as long as you’re not allergic; otherwise, you’d use Hibaclens.
I’m able to go ahead and place my probe back exactly on that spot. I can see exactly where I want to be. I pre-plan and make sure I’m in the proper area and proper plane. You can see I’m tilting the probe back and forth to optimize my image. Then I’m able to pre-plan where I’m going to go in, keeping my hand very stable so I’m not moving around.
I’m watching my image so I can get to the exact spot I want. You do not want to be watching your needle at this point, that would not be good. You want to see where you’re going; that’s the whole point of imaging. As you can see, I’m now advancing and getting to that subacromial space, dissecting along the region to open up that area and space, making sure I’m not too deep into the tendon. I’ve rechecked myself; I don’t want to bring my unit down on top of my needle which would contaminate the needle. I’m always keeping that hand steady; keeping my fingers on the patient; making sure I don’t move around that much; and I don’t contaminate my area. So basically, using the same sterile technique as I would for any surgery.
This one took a little bit longer because normally I would go in, just inject, and get out. As I said, we had to hydro dissect that region because of the adhesions, but this works very effectively for him and again, something that I wouldn’t really want to do unless I was using imaging. »
Bringing Ultrasound to Your Practice is Affordable
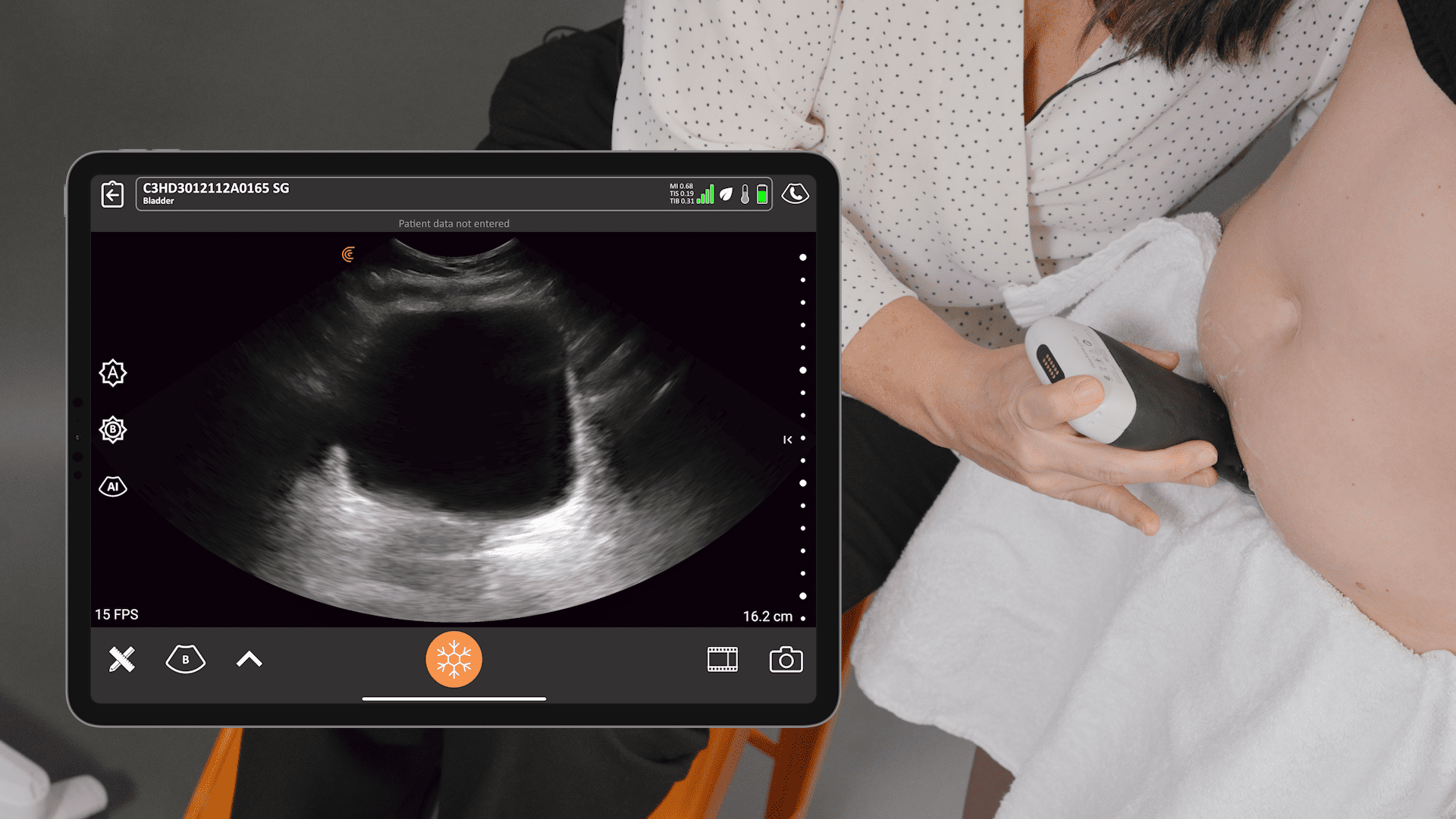
« It’s a myth that ultrasound costs too much. In fact, implementing ultrasound can be cost-effective and will improve your reimbursement. You may actually make more money on this, to be honest. The Clarius L15, for example, is very affordable, especially for the quality you’re getting. Visit the website to see published prices.

The images from the Clarius L15 are great on my iPad. I can see anatomy very clearly, and I’ve been very satisfied with it. What’s also nice is that if you aren’t confident, you can always use the Needle Enhance.”
Handheld Ultrasound for Orthopedic Surgery
Dr. Hirahara has been using Clarius wireless ultrasound since the first generation was introduced in 2016. As a member of the Clarius medical advisory board, he has helped optimize Clarius for orthopaedic treatments. Visit our orthopaedic surgery specialty page or contact us to learn more about why Clarius is the right handheld ultrasound for your practice.